Cardioversion and defibrillation
The application of electricity to the heart is capable of generating depolarization of the cells of the myocardium, resulting in interruption of the input circuits that induce cardiac arrhythmias. The objective of this depolarization is to get the sinus node into heart rhythm and thus fulfill its physiological pacemaker function.
Cardioversion and defibrillation techniques are relatively simple, but extremely dangerous for both doctor and patient if not performed correctly. Although the two techniques are similar, their indications, timing and the voltage of the current used are different.

Public domain

On the one hand, cardioversion is administered at a lower voltage and in a synchronized manner, that is, the equipment will induce electrical current to the heart at the moment the R wave is detected in the electrocardiogram. While defibrillation is a more drastic method, with a higher voltage and without the need to be synchronized.
Public domain Flickr
The heart
Anatomy
The marvelous organ called heart is located inside the thoracic cage in the middle of the lungs behind the sternum and in front of the dorsal spine. Its function is basically summarized in that it behaves as a physiological pump capable of beating 100,000 times a day (capacity to contract and relax) distributing sufficient blood to all the organs of the human body.
The heart, despite its important function, weighs approximately 200 to 400 grams, with the size of a closed fist. It is divided into 4 chambers, two lower ones called the right and left ventricles, which are larger and thicker in wall than the upper chambers called the left and right atria. Between these cavities there is a muscular wall that represents the septum and divides them into right and left ventricles and atria.
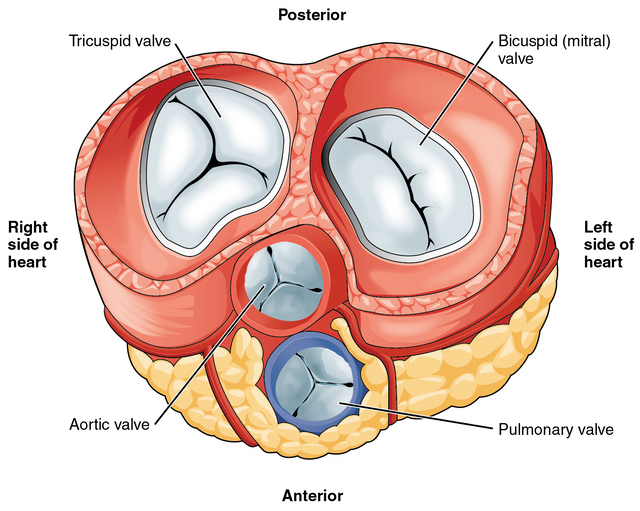
There are some small structures in these cavities whose function is to regulate blood flow, among which we have the tricuspid valve (between the right ventricle and the right atrium), mitral valve (which allows the passage of oxygenated blood coming from the lungs to the left atrium and ventricle), pulmonary valve (allows oxygen-free blood to pass into the lungs to be oxygenated from the right ventricle to the pulmonary arterioles) and finally the aortic valve (allows oxygen-rich blood to exit from the left ventricle into the major circulation to be distributed throughout the body).
Heart conduction system
Multiple synchronized electrical impulses are generated in the heart which stimulate the heart to contract. This electrical signal originates in the sinoatrial (SA) node located in the upper part of the right atrium, which plays the role of natural or physiological pacemaker. From this point, the impulses spread through the muscle fibers of the atria and ventricles in an orderly fashion and at a certain speed, causing the atrial depolarization and consequently its contraction.

Electrical conduction system of the heart. Public domain CC BY-SA 3.0
This electrical wave is then directed to the atrioventricular (AV) node at the level of the interatrial septum, from this area the impulse spreads through the fibers of both the right and left His bundle, where the latter is subdivided and distributes the impulse to the ventricles by means of a network of fibers called Purkinje fibers that trigger ventricular contraction.
Indications
Cardioversion
This method is carried out both electively and urgently, when medical therapy has failed and the patient cannot enter sinus rhythm. Usually the rhythm disorders where it is used are; reentry tachycardias (supraventricular tachycardia, atrial fibrillation, atrial fluter and Wolf-Parqkinson-White syndrome) these are usually associated or appear after acute myocardial infarction, cardiac angina, congestive heart failure, dyspnea, hypotension, syncope, acute lung edema and cardiogenic shock.
Defibrillation
Its indication is very specific, in cases of ventricular fibrillation or ventricular tachycardia without response to pharmacological therapy. Or in those cases where the patient is without peripheral pulse, unconscious, in apnea or during the advanced life support protocol.
Ventricular fibrillation or ventricular tachycardia secondary to myocardial ischemia, electrolyte imbalance, long QT syndrome, hypothermia or pharmacological intoxication (digoxin, tricyclic antidepressants, antihistamines, macrolide antibiotic combinations) may become a more stable rhythm following defibrillation.
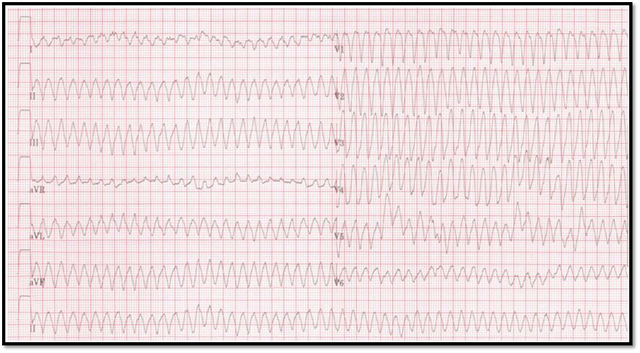
Ventricular flutter 12lead. Public domain CC BY-SA 3.0
Contraindications
Cardioversion
We should not attempt elective cardioversion in atrial fibrillation unless it is not known with certainty that it started within the last 48 hours and does not respond to drug therapy, that is, if it is a chronic A.F. it should not be cardioverted.
It should be avoided in patients with digoxin intoxication since in these cases it is ineffective, since the arrhythmias induced by these drugs are usually ventricular fibrillation or ventricular tachycardia.
Defibrillation
There are very few contraindications, the main one being that the patient in his right mind decides that he does not want to be resuscitated. Defibrillation should not be used in arrhythmias other than VF or VT.
All standard defibrillation/cardioversion units perform both of these maneuvers, and the new models have lower electrical output potentials for use with children. These devices are connected to a standard electrical source, and with rechargeable batteries, allowing this equipment to be portable. They also have a continuous paper-based electrocardiographic rhythm (ECG) recording.
In addition, this unit has a depolarizer which provides a direct electrical current useful in cardioversion and defibrillation, as well as, we can count on a synchronizer that allows the discharge of electrical current to be executed based on the shape of the electrocardiographic recording wave, in this case the unit looks for the trace of the R and S wave in the ECG to determine the moment of the current discharge.
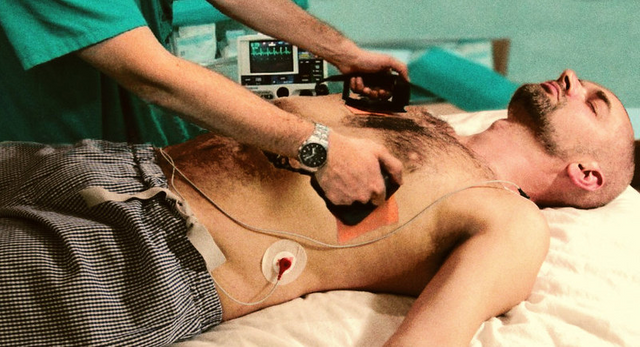
The paddles should be placed firmly and securely on the patient's torso. The recommended position is the anterolateral one, where the anterior paddle is located at the top of the right sternal border between the second and third intercostal spaces, while the lateral paddle is located between the fourth and fifth intercostal spaces at the midaxillary line.
)
Defibrillator Monitor Closeup. Public domain CC BY-SA 3.0
Preparing the patient
The patient is placed in a supine position, in a free area with the heart rate monitor, blood pressure and pulse oximeter along with oxygen at hand and as close as possible, without generating obstruction.
The patient must have at least one peripheral venous line before performing the technique. Have an aspirator and resuscitation equipment available if necessary.
These procedures are feared and above all painful for the patient, therefore, if there are no contraindications in the patient, prior intravenous sedation is recommended and the choice of sedative drug is up to the treating physician, however the most used are midazolam, propopol, thiopental, ketamine among others. The use of diacepam and loracepam has been reduced since they take time to start their sedative effect.
Technique
With the patient in the supine position and on the left side, the defibrillation/cardioversion unit is switched on. Connect the quick view mechanism of the paddles and place the ECG electrodes on the patient.
Always hold the left paddle (sternum) with the left hand and the right paddle (apex) with the right hand, in this way the anterolateral position of the paddles is achieved.
Once the paddles have been placed on the patient's chest and the line and rhythm have been observed on the cardiac monitor, the desired mode will be connected, i.e. non-synchronized if what is desired is defibrillation or synchronized if what is desired is cardioversion, based on the indications already described above. For example, in the case of ventricular fibrillation, the unsynchronized mode is induced, and therefore the defibrillation is required.
The energy to be applied must be indicated on the unit, if applicable:
We must be careful, the person who is going to execute the electric shock on the patient must ensure that his body is not in direct contact with the patient or the stretcher.
We proceed to execute the discharge in the desired mode according to the arrhythmia that the patient presents either cardioversion / defibrillation, at the end of the first shock should be observed the patient's heart rate on the monitor and perform an ECG, and check whether there is a need or not for a second shock.

Reanimation. Public domain CC BY-SA 3.0
Complications
Thermal and electrical burns are potential injuries in these cases, their incidence increases based on the energy used and the number of discharges made, as well as their severity and involvement of the skin layers. Occasionally, high blood pressure, other heart arrhythmias, or AV blockage may develop. You should always observe the monitor and see what the patient's heart is doing so that you can perform the cardioversion or defibrillation correctly and ensure that the shock that will be applied is highly necessary.
We must bear in mind that if the T wave is large and prominent, the electrodes must be adjusted so that the T wave is smaller than the R wave and so that the equipment does not deliver the electrical shock for a vulnérale and incorrect period, since if this is the case, and the shock is produced on the T wave, we could trigger a ventricular tachycardia since what we would previously be performing is a cardioversion.
Elevation of the CPK enzyme can be observed and this is mostly due to muscle injury and not myocardial ischemia.
Systemic emboli can occur from the ears of the atria if the patient's course is atrial fibrillation.
The paddles of the unit should not be placed directly on an implanted defibrillator or pacemaker as the electrical shock to be induced may permanently damage this device, which is why the position of the paddles is readjusted in these patients.
Avoiding injury to oneself or to the personnel working during the execution is the right thing to do, since otherwise this could generate burns in the area where the medical personnel come into contact, or worse still, trigger cardiac arrhythmias that you did not have previously.
Sources:

steemSTEM is a project of the chain of blocks that supports the scientific content in different areas of science. If you want to know more about this wonderful project you can join the server in discord
This article will be published at https://www.steemstem.io/
link
If you have any questions about any topic of medicine or present any disease you can comment the publication or write me in discord and I will attend you.
Dr. Ana EstradaI hope you enjoyed my content.
Your post has been curated by the bitcoin myk project. Tokens are available for this account you can trade for steem at: https://steem-engine.com/. Join our curation priority list to earn more tokens by registering at:
https://www.bitcoinmyk.com/register/
post in our steem group earn double the amount of tokens at: https://www.bitcoinmyk.com/social-media-2/
Visit our discord at: https://discordapp.com/channels/523971711733858364/523971711733858366
Bitcoin MYK
admin
Register - Bitcoin MYK
This post earned 50 BTCMYK
Thank you very much
Dear @anaestrada12, great explanation about the application of electricity to the heart and the parameters of well use of this strategy. Cheers!
@tipu curate
Upvoted 👌 (Mana: 0/20 - need recharge?)
Thank you @ritch I'm so glad you liked the topic.
Cheers ;)
This post has been curated by Steemitas Club. Congratulations @anaestrada12 and thank you for sharing this original work.
If you are not a member of @steemitasclub, we cordially invite you to join our discord server (https://discord.gg/dYMsF7a) to promote your publications. Steemitas Club is a community to give free delegations to new steemians and also has a curation project to support original content.
Thank you @steemitasclub
Thanks for another informative post.
I think you're referring to Propofol here. :)
Are you really only doing the AL position when you try to do a conversion?
I once witnessed an AP application also when I did an internship at anaesthesia care 2 years ago - a quick look at the papers suggests that both are common. But I only know the German way. ;)
Greetings, @isarmoewe I hope you are well, if what is referred to is propofol, it is an insurance error at the time of transcription. Thank you for reading the article
This post has been voted on by the SteemSTEM curation team and voting trail. It is elligible for support from @curie and @minnowbooster.
If you appreciate the work we are doing, then consider supporting our witness @stem.witness. Additional witness support to the curie witness would be appreciated as well.
For additional information please join us on the SteemSTEM discord and to get to know the rest of the community!
Thanks for having used the steemstem.io app and included @steemstem in the list of beneficiaries of this post. This granted you a stronger support from SteemSTEM.
Thank you very much @steemstem