Type 2 Diabetes - from the eyes of immune cells.
Genetics and lifestyle. That are the two quick answers that you get when you ask - the causes of type 2 diabetes. However, there is no denying that they do play a role. While certain genes can increase your risk of being diabetic, your lifestyle can be a fuel to it. But that picture is far from complete. To device the best lifestyle choices and to find the most effective cures it is necessary to understand whatever happens in between. To be more specific what drives the progression of a person from being healthy, to developing insulin resistance, and eventually compromising insulin production. Well the road to pathogenesis of diabetes is not a straight broadway. It is a rather complicated network of events. In this series about diabetes, I will focus on exactly that. I will pick one node at a time and discuss its contribution to pathogenesis of type 2 diabetes. In conclusion of the series I will try to connect the dots and see how it all works together. Today I will specifically talk about how chronic inflammation is at the central hub in onset of type 2 diabetes.
Mechanism of type 2 Diabetes.
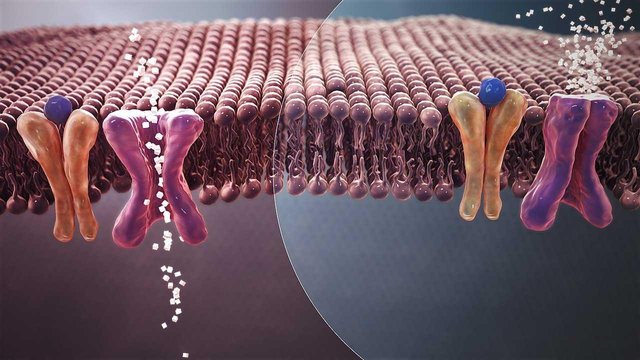
Left - In cells of healthy people the Insulin(blue) binds to insulin receptor. This causes cells to open their glucose transporter and take up glucose. Right -Cells of diabetic patients don't respond to insulin and don't take up glucose.
Source
Author Manu5
CC Attribution-Share Alike 4.0
A brief history Diabetes
I don't doubt that you might already know what diabetes is all about. Nonetheless, it doesn't hurt to have a brief recap, so everyone is on the same page. So let's get done with this boring part really quick.
The sugar(glucose) is the fuel your cells needs to burn to make energy. So every cell in body kind of needs that. Nonetheless, being a multicellular organism means that you need to tell all cells to behave like a good society. Which means the uptake of glucose is regulated by the body. On the other hand cells have mechanisms to control how much glucose they will take in(just like you put that plate down when your hunger is satiated). When we eat food, our pancreas sense that there is a rise in level of glucose in blood, the β-cells in pancreas respond by secreting insulin. Insulin is a hormone, which goes and bind to insulin receptors (proteins on cell membrane that sense molecules in cell surroundings) on other cells. In response, the cells open their glucose transporters and take up glucose from their surroundings.
Now imagine two situations. First, a situation where the β-cells are compromised and insulin secretion is highly reduced. And second one in which the insulin receptors on the cells are reduced in number, or desensitized in responding to insulin. In both situations you end up with cells not taking up enough glucose from the blood. This is what diabetes is about, inability of body to use circulating glucose. The high blood glucose level then causes all known secondary maladies of diabetes - such as neuropathy, rentinopathy, vascular defects and cardiac abnormalities.
If this inability in using glucose is due to immune system attacking β-cells and killing them in early age you can term it as insulin dependent or type 1 diabetes. Type 2 diabetes is majorly adult onset and starts with cells of the body becoming resistant to insulin. The insulin resistance raises the blood glucose levels, eventually telling your β-cells to produce more insulin. The high blood sugar level puts a constant demand for producing more insulin. This eventually stresses the β-cells and kills them, worsening the disease even further. So in later stages of type 2 diabetes you are not only resistant in responding to insulin but you also stop producing it. But why do these cells become resistant to insulin, and what kills the β-cells? For today I will put both these blames on immune cells and you will see why.
Diabetes as an inflammatory disease.
What if I told you that type 2 diabetes is not just a lifestyle but an inflammatory disease? If I were you I will quickly go ahead and ask - so is there a correlation between a chronic systemic inflammation, and onset of insulin resistance? The answer turns out to be yes.

Inflammation - the hub between known risk factors and onset of type 2 diabetes.
Created by @scienceblocks
Chronic inflammation - the oracle predicts your fate.
We should have started looking at diabetes as inflammatory disease back in early 1900s when in 1876 Ebstein and later Williamson in 1901, used Salicylate to treat diabetes. But better late than never. The interest was reignited in 1990s. In 1999, Schdmit et al., established that markers of inflammation can be used as risk predictors for type 2 diabetes. Then just a few years later Schmidt co-authoed yet another paper with Duncan and colleagues; where they show that chronic low-grade systemic inflammation was common in people who developed diabetes in their 9 years of follow up. This began a quest of discovering the role of immune cells, and inflammatory cytokines(molecules secreted by immune cells) in type 2 diabetes onset. But in this quest the first and the foremost thing is to establish that inflammation is indeed a cause of type 2 diabetes, rather than merely being correlated with it. Now most of this research comes from over eating obese mice and this is where we are going to ponder for a while.
How obesity narrated the link between inflammation and diabetes.
db/db mouse model for diabetes
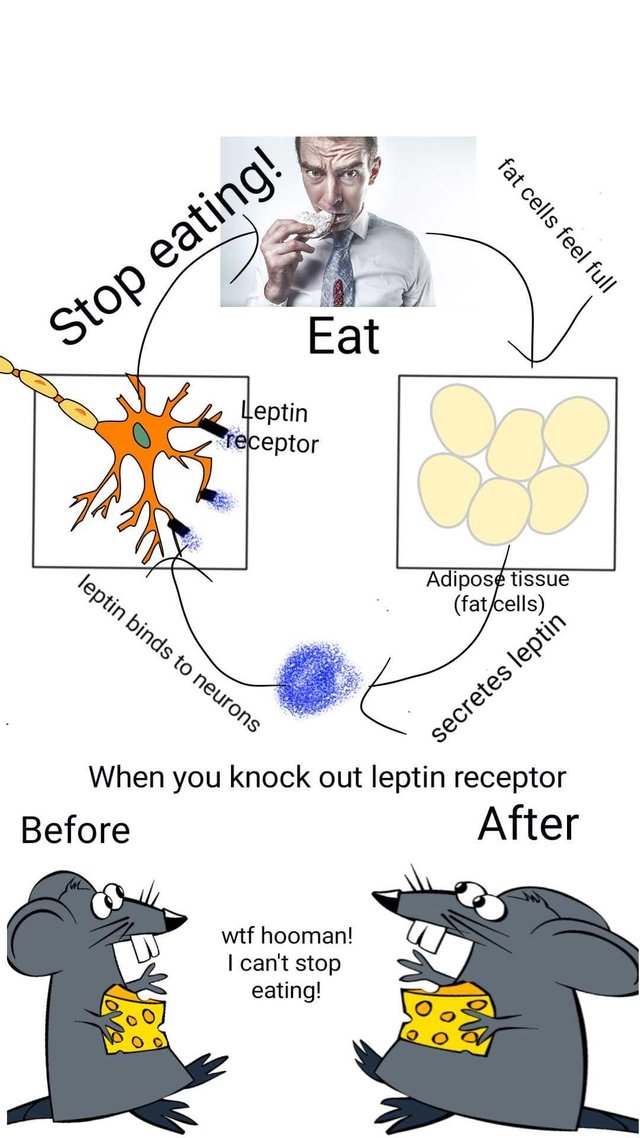
Leptin is a hormone that maintains the energy balance in the body. It is secreted by fat cells proportional to their fat content. The leptin binds to neurons in brain and inhibit hunger. Now if you remove or mutate leptin receptor in the brain or gene for making leptin, it would lead to an insatiable hunger. The db/db mice have mutated Leptin receptor. They eat ferociously and become obese. This also leads them to develop human type 2 diabetes like condition. Alternatively, you can make a genetic mutant that does not produce leptin hormone. This is ob/ob mice, which is another model for studying obesity and type 2 diabetes.
Sources:
neuron
Fat cells
mouse eating cheese and modified fat version of it
Human eating cookie
CC0
The classical model used in research is a db/db mouse. This mouse has a mutated Leptin receptor, which causes it to over eat, leading to development of obesity, and insulin resistance. It has been shown time and again that there is a causative link between these mice developing inflammation and hence insulin resistance.(Lee et al., 2010). Based on this you may predict that anti-inflammatory drugs should reverse or at least improve the insulin sensitivity in these mice. Consistent with this prediction, salicylates such as aspirin do seem to have a protective effect in db/db mice(Yuan et al., 2001). Moreover, if you make a transgenic mouse that overexpress IL37(an anti-inflmmarory protein), and cross it with db/db diabetic mouse model, it rescues insulin sensitivity in this cross(Ballak et al., 2014).
Fair enough! However, one might argue that it wasn't just inflammation but obesity in these mice and people that also contributed to diabetes. Moreover, the interesting aspect of this whole obesity - inflammation - insulin resistance fiasco is that it is a two way feedback. So while fat stimulates immune system and causes insulin resistance, the insulin resistance can promote inflammation and obesity as well. Which makes one question, the individual contribution of obesity and inflammation in pathogenesis. Now, it is known that macrophages in adipose tissue of the obese mice secrete a pro-inflammatory molecule, TNF-alpha, so what happens if you knock it out or block it in dB/dB mice? Well, It did protect the mice from developing insulin resistance(Uysal et al., 1997). Instead of using a genetic model for obese mice you can use a mice fed using high fat diet and replicate the same results with TNF-alpha. You can as well delete the gene for JNK1 in hematopoietic cells(an important gene in progression of type 2 diabetes) and you will find that adiposity alone is not sufficient to induce insulin resistance in absence of inflammation(Solinas et al., 2007). Moreover, you can also test this hypothesis by overexpressing an implicated inflammatory cytokine such as IL6 in mice, and the mice will develop insulin resistance(Franckhauser et al., 2008).
We know that obesity is major risk factor associated with type 2 diabetes in humans, as well. Salicylates has already hit the clinical trials and they seem to improve both insulin resistance and insulin secretion in type 2 diabetes patients(Fang et al., 2008). How exactly obesity promotes inflammation may still require more research. However, quite a few hypothesis have been proposed. For instance, since amount of adipose cells needs to be increased for increasing amount of nutrients, the excessive adipose tissue may promote hypoxia which causes more immune cells to infiltrate. Then free fatty acids in obese people may also contribute to promotion of inflammation.(See Ellulu et al., 2017 for more.) Yet another possible mechanism is decrease in the amount of the suppressor cells. For instance, T-regulatory cells are decreased in adipose tissue of obese people(Feuerer et al., 2009). And infact reinjecting heathy Tregs is a proposed treatment for type 2 diabetes. Nevertheless, obesity is not the only risk factor for diabetes. I mean ofcourse chronic inflammation, as well, is not only caused by obesity. So let's ask if inflammation is correlated with other risk factors of type 2 diabetes as well.
Diet - what you eat matters
The vicious cycle of fatty foods, inflammation and more food.
We already saw that mice fed on high fat diet is a non genetic model of type 2 diabetes. It appears that some fatty acids bind to TLR4 receptors on immune cells, which is a classical receptor for binding lipopolysaccharide (LPS) from bacteria. The cool part is if you remove TLR4 gene from mice, you may still make them obese, but they will be protected against insulin resistance(Shi et al., 2006). Hypothalamus, a region in brain that tells you to stop eating when you are satiated, seem to be a direct target of fatty acid induced inflammation. Fatty acids do lead to inflammation of other organs as well(Sears and Perry, 2015) but hypothalamus is interesting, because inflammation in this part make you lot like db/db mice. So the more of these saturated fatty acids you eat, the more you might lose control on when to stop eating.
Sugars - looks like immune cells are fugivores
Eating excessive sugars, and drinking those sugar concentrated sodas have been linked to insulin resistance. Nonetheless the major debate has been whether it just the amount of caloric intake or is any specific sugar more evil - fructose, glucose or sucrose(a disaccharide of fructose-glucose)? From the perspective of this article which sugar, if any can cause inflammation and hence insulin resistance? Fructose seems to be the major culprit when it comes to making you fat and diabetic. High fructose diet over long period lead to increased free fatty acids, VLDL and plasma teigycirides. All of which are known to be pro-indlammatory and for their contribution to insulin resistance. Eventually high fructose diet leads to chorionic inflammation in adipose tissue(Zhang et al., 2017).
Ageing
Not every old person becomes obese. Nonetheless ageing increases the risk of developing type 2 diabetes. The major contributor to age related risk of insulin resistance yet again appears to be increase in chronic low grade inflammation in adipose tissue(Wu et al., 2007, Brüünsgaard and Pedersen., 2003)
Physical activity
Now, it would be weird to imagine that body punishes you for not giving it enough excercise. However it does appear that physical activity reduces the inflammation and improves insulin sensitivity(Venkatasamy et al., 2013).
Stress and Mental health
If you look closely at NIDDK article, you will find that depression is listed as risk factor for developing type 2 diabetes. Though the results in this regard are preliminary, but both depression and type 2 diabetes, share common inflammatory markers(Doyle et al., 2013). Also, it known that chronic stress is linked with low grade chronic inflammation. It is not surprising that psychological stress is also a predictor of type 2 diabetes(Liu et al., 2017).
Viruses and type 2 diabetes
If chronic inflammation does contribute to onset of type 2 diabetes, you may predict that chronic virus infection may predict that as well. For instance in this study a chronic hepB infection predicted insulin resistance. Moreover it will be even worse for obese people to get infected by a virus. A virus infection may just accelerate the onset of type 2 diabetes. This prediction is infact in line with a recent study, published a this month. In this study the virus induced interferon gamma, which induces insulin resistance. The insulin resistance led to hyperinsulinemia, which hyper activated CD8+ T cells. These cells are anyway known contributors to insulin resistance. The poor mice as a result got a boost towards diabetes.
Thinking of it, immune cells are there trying to help you. Macrophages clearing fat from adipose or be it these T cell fighting viruses. However, if the underlying issue is not resolved in time the price of this help could be type 2 diabetes. In fact, I would have loved to talk about contribution of different immune cells in type 2 diabetes. But, I suppose that there comes a time in life of every article when it should stop. I mean I can go on talking about it, but I decided to not stretch your attention span. For now let's end this at the note that unwanted chronic inflammation does link environmental factors to type 2 diabetes. I will explore yet another node of diabetes pathogenesis in this series next week.
References
A special thanks to @deathbatter another steemSTEM author, since our disscussion in comment section of his blog inspired me to start this series. I hope everyone will find it informative and enjoyable.
Signing off
@scienceblocks

Resteemed your article. This article was resteemed because you are part of the New Steemians project. You can learn more about it here: https://steemit.com/introduceyourself/@gaman/new-steemians-project-launch
Good article, thanks for this! What do think harms more? Eating sugar or eating? Greetings, Chapper
Posted using Partiko Android
More than sugar vs fat, it is about which sugar vs which fat. What might be healthy for one person also depends on their geographic and genetic background. In fact a paper published in Cell in 2015 showed that same food causes different metabolic responses in individuals. So honestly diet has to be personalized. If banana is poison for one, it may be healthy for me. But if you ask my opinion, from most research it appears to me that sugars, specifically fructose is major culprit. In fact following these papers I was able to lose 10 kgs within 2 months when I went on low carb high fat diet. I think until one finds a personalized regime for healthy diet, lowering sugar intake to minimal requirement would be best. I would call the synergy of sugar and fat most deadly, like Ham burgers as daily meal might be a really bad idea.
Hey @scienceblocks
Here's a tip for your valuable feedback! @Utopian-io loves and incentivises informative comments.
Contributing on Utopian
Learn how to contribute on our website.
Want to chat? Join us on Discord https://discord.gg/h52nFrV.
Vote for Utopian Witness!
Fat, sorry 😉
Posted using Partiko Android
Congratulations! This post has been upvoted from the communal account, @minnowsupport, by scienceblocks from the Minnow Support Project. It's a witness project run by aggroed, ausbitbank, teamsteem, theprophet0, someguy123, neoxian, followbtcnews, and netuoso. The goal is to help Steemit grow by supporting Minnows. Please find us at the Peace, Abundance, and Liberty Network (PALnet) Discord Channel. It's a completely public and open space to all members of the Steemit community who voluntarily choose to be there.
If you would like to delegate to the Minnow Support Project you can do so by clicking on the following links: 50SP, 100SP, 250SP, 500SP, 1000SP, 5000SP.
Be sure to leave at least 50SP undelegated on your account.
Congratulations,
you just received a 20.46% upvote from @steemhq - Community Bot!
Wanna join and receive free upvotes yourself?
Vote for
steemhq.witnesson Steemit or directly on SteemConnect and join the Community Witness.This service was brought to you by SteemHQ.com
This post has been voted on by the steemstem curation team and voting trail.
There is more to SteemSTEM than just writing posts, check here for some more tips on being a community member. You can also join our discord here to get to know the rest of the community!