Antibiotic Resistance - A Growing Health Concern #3 - Quinolone Resistance
It is a growing concern in the medical world. Microbes are developing more and more antibiotic resistances and due to the long process of trials and testing we may run out of effective antibiotics. Many only know the term antibiotic resistance and the consequence, but what about the mechanism? This is the third post in this mini series about antibiotic resistance. I will post every Tuesday explaining different mechnisms by which microbes become resistant to bacteria. Today I will talk about resistance to quinolones.
Other Posts In This Series
- Antibiotic Resistance - A Growing Health Concern #1
- Antibiotic Resistance - A Growing Health Concern #2: Penicillin Resistance

What Are Quinolones And How Do They Work?
Quinolones are a type of antibiotics and not very similar to the beta-lactam based antibiotics I wrote about last week (as you can see in the picture below).
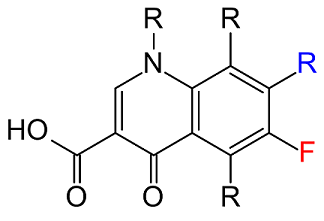
Quinolones comprise several chemically-related substances, which all have 3-carboxyl and 4-carbonyl functional groups, which are able to bind DNA (1). Their origin dates back to the discovery of nalidixic acid in 1962, but it was not until the discovery and licensing of fluoroquinolones in the 1970s and 1980s that these antibiotics became widely used (2). Fluoroquinolone usage rapidly increased in 1990 and they became the most prescribed antibiotic in 2002 (3). They action is making use of the fact that bacterial DNA replicating enzymes differ from human DNA replicating enzymes (4). Quionolones trap DNA gyrase and DNA topoisomerase IV on DNA, which basically disrupts DNA replication in bacteria (5), slowing down their growth rate and eventually leading to cell death. Quinolones can bind either enzyme, but sensitivity varies in Gram-positive and Gram-negative bacteria (6). Thus quinolones can be used as broad spectrum antibiotics against several diseases such as anthrax, tuberculosis, bacterial pneumonia, and sexually transmitted diseases (7). They are usually given orally, spread throughout the body and are broken down by either liver or kidney and then excreted in our urine (9).
Mechanisms Of Resistance
A mechanism that has attracted considerable attention is a mutation in topoisomerase IV. A recent study states that a mutation at the serine 81 residue of Bacillus anthracis topoisomerase IV prevents the formation of a water-Mg 2+ bridge between the enzyme and quinolone, thus decreasing the affinity of the enzyme for quinolone (10). Another study has come to a similar conclusion, but mentioned a mutation in another amino acid residue, glutamic acid 85, as a cause for a disrupted water-Mg 2+ bridge (11). Both studies stated that either more potent quinolones, or higher Mg 2+ concentrations can overcome this mechanism and reverse resistance (10), (11). This is an example of a vertical acquisition of resistance, as a mutation in one cell is passed on to the descendents.
.svg.png)
Another type of resistance spread is horizontally, where genetic material is spread in the form of plasmids (small rings of DNA separate from the "main" circular DNA in bacteria) between bacteria (4). These plasmids commonly contain genes that encode so called Qnr proteins, which are able to protect DNA and the two target enzymes from quinolones (12). Another protein that is spread by plasmid exchange is aac(6′)-Ib-cr, a modified aminoglycoside acetyltransferase, which is capable of acetylating the unsubstituted nitrogen of the C7 piperazine ring, decreasing the effectiveness of some quinolones (13). Yet another mechanism transferred with plasmids is expression of genes expressing certain specific efflux pumps, which specifically pump quinolones out of the cell (14).
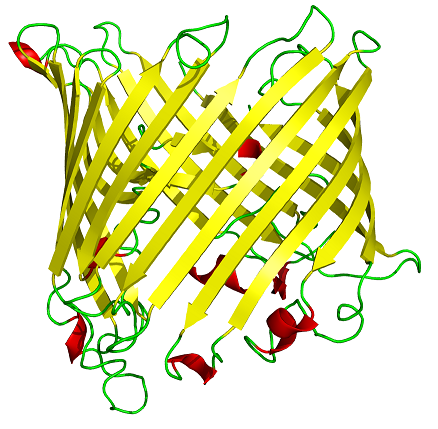
Another, non-specific mechanism is the downregulation of porin-production, which I already talked about in last week´s post. However, here is an illustration of a porin again (people seemed to like it).
It appears that the most important mechanism of resistance is based on the mutation of amino acid residues at the target enzymes (13). The other mechanisms likely contribute to the selection of vertically acquired resistances (12). This is supported by the observation that resistances first occured in species where a single mutation resulted in clinically sufficient resistances, whereas other specied required multiple mutations to acquire clinically significant resistance (15). Sadly this has even more serious implications. Many bacteria that are resistant to quinolones are also resistant to other antibiotics, which means they are multiresistant (16).
Summary
Bacteria acquire resistance to quinolones mainly by mutations at specific amino acid residues in the enzymes gyrase and topoisomerase IV. These mutations decrease affinity towards quinolones. Other mechanisms include acetylation of certain quinolones as well as production of specific efflux pumps. Non-specific porins can help to keep the concentration of quinolones in the cell below effective levels. Some bacteria require multiple mutations to acquire clinically significant resistance, whereas others can be resistant with only one specific mutation.
Shameless Self-Advertisement
Thank you very much for reading today´s antibiotic resistance post. I hope that you learned something new about the mechanisms that lead to microbial resistance to one of the most common class of antibiotics - quinolones. If you liked this post, please upvote and resteem.
Please let me know if I made mistakes or left something out. Especially for today´s post as I was feeling a little drowsy while writing this (bacteria got me - in short, I am sick).
As always,
Cheers @lesshorrible!