Antibiotic Resistance - A Growing Health Concern #2: Penicillin Resistance
It is a growing concern in the medical world. Microbes are developing more and more antibiotic resistances and due to the long process of trials and testing we may run out of effective antibiotics. Many only know the term antibiotic resistance and the consequence, but what about the mechanism? This is the second post in this mini series about antibiotic resistance. I will post every Tuesday explaining different mechnisms by which microbes become resistant to bacteria. Today I will talk about resistance to penicillin.
Other Posts In This Series

What Is Penicillin And How Does It Work?
Penicillin was discovered by Sir Alexander Fleming when he observed that a mold secreted a substance that prevented bacteria from growing on a medium (1).
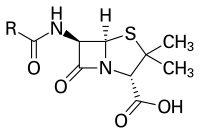
Core - Source
It first was isolated by Howard Florey and Ernst Boris Chain in the late 1930s, and by 1941 the first injectable treatment became widely available (2). Penicillin is able to bind to an enzyme, transpeptidase, which is responsible for crosslinking the sugar-peptides that form the peptidoglycan cell wall of bacteria (3). Penicillin acts as a structural analog of the acyl-D-alanyl-D-alanine terminus (4). The ring structure you see in the picture on the left is called beta-lactam. It is a reactive species which makes penicillin so powerful. Since it is structurally so close to the natural substrate, transpeptidase recognizes penicillin as its substrate, binds it, and due to the reactivity of the beta-lactam ring, penicillin reacts and alters the active side of the enzyme. Enzyme function is structure-dependent, so even slight changes may make an enzyme inactive (5). However, almost immediately after the introduction of the first antibiotic in the 40s the first resistances were observed, and by the end of the 50s the previous advances in the fight against bacterial infections were almost lost (6). So how are microbes resistant to penicillin? I will no talk about the two most common mechanisms by which microbes have become resistant to penicillin.
Two Main Mechanisms
The first generation of antibiotic resistant microbes developed a mechanism that destroyed what has destroyed them. They acquired the ability to produce an enzyme, which is able to hydrolyze the amine bond in the reactive beta-lactam ring, making penicillin ineffective (7). There are as many as 850 known beta-lactamases (8). This shows how wide-spread resistance to penicillin-based antibiotics are. Luckily, the structure of penicillin can be changed while maintaining the reactive beta-lactam ring. If you go back to the structure of penicillin, you will notice a group labelled “R” in the left corner. This means that there can be some different groups attached here. A modulation of penicillin is the addition of bulky groups, which result in steric hinderance of the beta-lactam ring (9). One penicillin-based antibiotic arising from this approach is methicillin. Methicillin has helped to overcome the penicillin resistance that arised in the 1950s (6). The development of methicillin and other antibiotics led a Nobel laureate to say: “One can think of the middle of the 20th century as the end of one of the most important social revolutions in history, the virtual elimination of the infectious diseases as a significant factor in social life” (10).
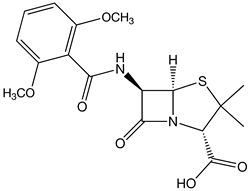
Sadly microbes have high rates of mutation and thus acquired resistances to methicillin (11). This has led to the development of another mechanism by which microbes have become resistant to penicillin-based antibiotics. Those microbes turn the tide and use a mechanism that is somewhat similar to the activity of penicillin. Methicillin-resistant microbes produce a peptide that can bind methicillin (12). On of those microbes is the staphylococcus aureus, which is the organism behind MRSA infections. Methicillin is not used clinically anymore (13).
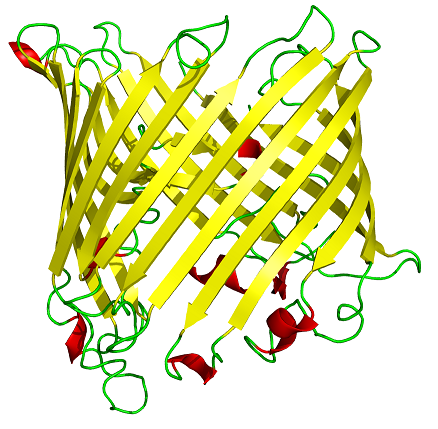
There is another, less specific mechanism. Many Gram-negative bacteria have porins in their outer membrane through which they can import a variety of substances (14). Porins are proteins that consist of an arrangement of three beta-barrels. Those are membranes that cross the outer membrane allowing substances to enter the periplasm (Gram-negative bacteria have an inner and an outer membrane with a cytoplam in between those membranes which is called periplasm). Some microbes decrease the production of porins as a response to the presence of antibiotics (15). This decreases the uptake of antibiotics which helps them to survive being subjected to antibiotics. It is not necessarely a resistence mechanism, however it helps microbes to decrease the effects of antibiotics on them.
Shameless Self-Advertisement
Thank you very much for reading today´s antibiotic resistance post. I hope that I was able to convey to you the basic mechanisms that result in mircrobial resistance to the first used antibiotic - penicillin. If you liked this post, please upvote and resteem.
As always,
Cheers @lesshorrible!
This is a test comment, notify @kryzsec on discord if there are any errors please.
Being A SteemStem Member
Super interesting and such an important topic, thanks for posting! I'm really not on good terms with antibiotics and have developed allergies quite a while ago after being treated with them for no good. Can't believe that they are still most doctors' go-to-response to any infection-like symptoms, even if they don't know if the symptoms are actually caused by bacteria.
What a colourful picture of sucrose porin! Honestly, mechanisms went above my head ;) I have to read it 3-4 times to understand :)