Urinary Stones : Understanding the basics
The term Urinary Stones, refer to stones anywhere in the urinary tract, starting from the nephrons in the kidneys to the major and minor calyces, to the renal pelvis, ureters and the urinary bladder.
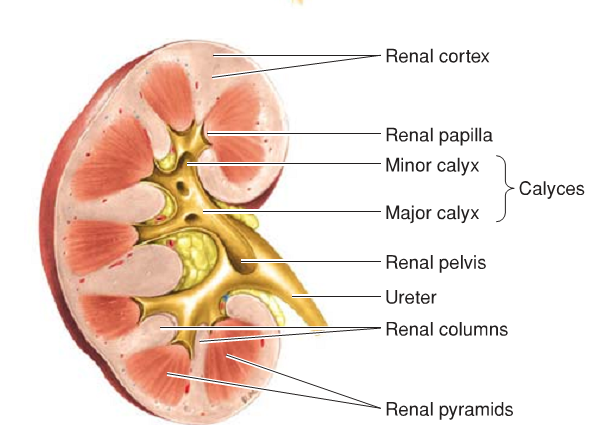
image from High Yield Gross Anatomy, 5th edition
What causes stones to be formed in the Kidneys and the Urinary tracts :
- Diet : Deficiency of Vitamin A causes desquamation of epithelium. The cells form a nidus around which a stone can be deposited.
- Increases concentration of urinary solutes : The most important factor for the increase in concentration of the urinary solutes is Dehydration. If theres less water available for the solutes to dissolve in, they'll precipitate out and form stones.
- Decreased Urinary Citrate : Citric acid tends to keep relatively insoluble calcium phosphate in solution. Decreased citrate thus increases the risk of the calcium phosphate to precipitate out and form stones. And thus supplementing citrate will be an important method in treating calcium stones (as we will see below).
- Renal Infection : When urine is infected with urease positive bugs like proteus mirabalis, staphylococcus saphrophyticus, klebsiella, they will hydrolyze urea into ammonia. This will make the urine more alkaline. Phosphate stones tend to grow in alkaline urine.
- Inadequate urinary drainage and urinary stasis: Whenever there is stasis, there is always an increased risk of solutes precipitating out as stones.
- Hyperparathyroidism: Leads to hypercalcemia, which will lead to more calcium in the urine, thus a higher concentration which as we have already seen tends to increase the risk of stone formation.
Classification of Renal/Urinary Tract Stones :
Based on the radiologic findings, there are 2 classifications :
- Radio-opaque: These are the stones that will be visible on radiography. 90% of the stones are radio-opaque.
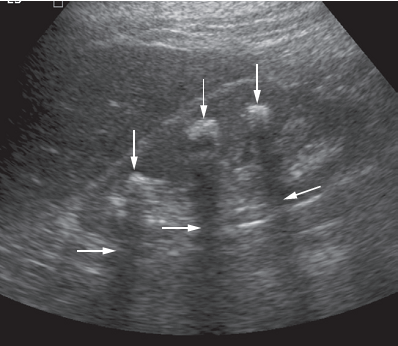
image from Diagnostic Imaging, 7th edition
- Radio-lucent: But we should not forget that 10% of the stones are not visible on radiographs and so a negative result on a radiograph does not exclude the diagnosis of renal/urinary tract stone.
Based on the composition, the 4 main classifications are as follows :
- Calcium Oxalate Stones (~60%) : These stones are irregular in shape. They are hard and covered with sharp, spiky projections which tends to cause bleeding. These stones are black or dark brown in color. Calcium Oxalate stones are radio-opaque and thus visible of radiographs. Treating with Thiazide diuretics and Citrate is helpful to reduce the stones.
The crystals are shaped as octahedrons.

image from First Aid
- Phosphate Stones (~33%) : Usually calcium phosphate, but sometimes can also be combined with ammonium and magnesium phosphate, especially if there is infection with protease positive microbes. These stones tend to be smooth and dirty white in colour. May initially be asymptomatic, but are visible on radiographs. These stones tend to enlarge over time if the infection is not eradicated and may enlarge to fill up the entire or most of the collecting system. When this happens, it is known as a Stag-horn Calculus.

image from First Aid
Eradication of infection is necessary to treat these type of stones.
The crystals look like this :
image from First Aid
- Uric acid and Urate Stones (~5%) : These stones are hard, smooth and often multiple. Color caries from yellow to reddish brown. Pure uric acid stones are radio-lucent. Often seen in diseases that cause hyperuricemia (for example, Gout) or has high cell turnover rate (for example, Leukemia).
Alkalinization of urine helps dissolve these stones. Allopurinol decreases synthesis of uric acid, so is a helpful drug to control uric acid stones. The crystals look like a rhomboid :
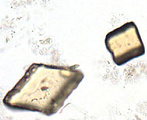
image from First Aid
- Cystine Stones (~2%) : Occurs in patients with Cystinuria, an autosomal recessive disease. Usually starts to appear in childhood and has the potential to form stag-horn calculi. The stones are hard and multiple in number. Pink or yellow in color when first removed, but changes to a greenish color on exposure to air. Treatment involves alkalinization of urine and use of chelating agents in refractive cases. The crystals are hexagonal :

image from First Aid
CLINICAL FEATURES:
- AGE: 50% of the cases present between 30 and 50 years of age.
- Sex: Male : Female ratios is 4:3
- Symptoms:
- The leading symptom in 75% of the cases is Pain. Depending on the location of the stone, the pain can be Renal Colic, which is a fixed pain located posteriorly in the renal angle, anteriorly in the hypochondrium or both, or the pain can be Ureteric Colic, which presents as agonizing pain passing from loin to groin. Ureteric colic is almost always associated with nausea and vomiting. If the stone is in the bladder, pain may occur at the end of micturition and is referred to the tip of the penis or to the labia majora or the medial side of the thigh which is worsened by movement. This type of pain is also known as stranguary.
- Hematuria
- Pyuria
- Uremia (this may be the first indication of presence of stones if the stones are bilateral)
- Interruption of the urinary stream and Sensation of incomplete bladder emptying (bladder stones)
- Increased frequency of urination, more common during the day (bladder stone)
- Some cases may be completely asymptomatic for long periods of time, even large stag-horn calculi, during which there may be progressive destruction of the renal tissue.
- Signs:
- Rigidity of the lateral abdominal muscles during an attack
- Tenderness and rigidity along the course of the ureters
- Tenderness in renal angle on gentle deep palpation
- Percussion over kidney produces a stabbing kind of pain
- Rarely, the kidneys maybe ballotable, if there is hydronephrosis (accumulation of water in the kidneys because the stones are obstructing urine outflow) or pyonephrosis (infection).
INVESTIGATIONS:
- General:
- Renal Function Tests : Blood urea, serum creatinine
- Blood for calcium and phosphate levels
- CBC (complete blood count)
- Blood sugar
- Routine urine examination and microscopy and culture
- Specific:
- Plain x-ray of the KUB (kidney, ureter and bladder) region : Opaque shadow for stone and enlarged kidney shadow
- Ultrasonography (USG) of the KUB region : Can detect and locate the position of most stones
- Retrograde Pyelography : Most precise imaging method to determine the anatomy of the ureter and renal pelvis and helps establish definitive diagnosis of ureteral stones.
- Excretion Urography : Radio-lucent stones can be detected by the presence of filling defect.
Stones not clearly visible
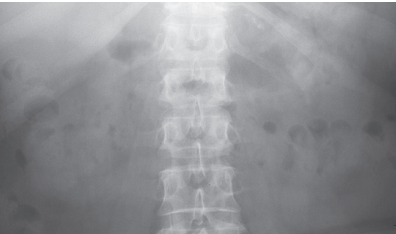
image from Diagnostic Imaging, 7th edition
Filling defect (arrows) shows the location of radio-lucent stones.
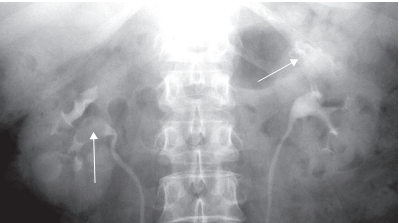
image from Diagnostic Imaging, 7th edition
TREATMENT :
- Symptomatic Treatment :
- Hydration : This is extremely important. Take in plenty of fluid, IV or oral. If you have had uncomplicated urinary tract stones in the past, staying well hydrated may help prevent recurrence.
- Bed rest
- Analgesic and Antispasmodic for pain
- Sedative
- Appropriate Antibiotics for urinary infection
- Treatment of uremia if present
- Removal of Stone :
Expectant Treatment : Small stones (<0.5 cm) are likely to pass spontaneously unless they areimpacted. The progression of the stone is followed by x-ray of KUB every 6-8 weeks.
Surgical removal :
Endoscopic surgery :
a) Percutaneous Nephrolithotomy
b) Extracorporeal Shock Wave Lithotripsy (ESWL)
c) Both in case of stag-horn calculi.Open Surgery :
a) Percutaneous Nephrostomy
b) Pyelolithotomy (when the stone is in the extrarenal pelvis)
c) Extended Pyelolithotomy (when the stone is in the intrarenal pelvis)
d) Nephrolithotomy (stone in calyces)
e) Partial nephrectomy (stone in the lower most calyx)
f) Nephrectomy (When one kidney is damaged or associated with severe infection and the other kidney is healthy)Treatment of Bilateral Renal Stone :
- Kidney with better stone is treated first
- In case of severe pain, the painful kidney is operated on first. Operation of the other kidney is done usually after 2-3 months.
Sources :
Bailey & Love's Short Practice of Surgery, 26th Edition
Diagnostic Imaging, 7th Edition
Medscape
First Aid for the USMLE Step 1
Alright guys, that's it for now!! Hope you learned something today!!
Start Upvoting to increase your Curation Rewards. Resteem this post and maybe more people out there might find this useful.
If you enjoy medical topics, health tips, or steemit tutorials for beginners and newbies, please make sure to follow me at @simplifylife
Peace!!
This post recieved an upvote from minnowpond. If you would like to recieve upvotes from minnowpond on all your posts, simply FOLLOW @minnowpond
Retracted
Thank you very much. I'm glad we could sort it out!! :)
Congratulations @simplifylife! You have completed some achievement on Steemit and have been rewarded with new badge(s) :
Click on any badge to view your own Board of Honor on SteemitBoard.
For more information about SteemitBoard, click here
If you no longer want to receive notifications, reply to this comment with the word
STOPThis post has received a 6.42 % upvote from @buildawhale thanks to: @simplifylife. Send at least 0.25 SBD to @buildawhale with a post link in the memo field for a portion of the next vote.
To support our curation initiative, please vote on my owner, @themarkymark, as a Steem Witness
This post has received a 0.54 % upvote from @booster thanks to: @simplifylife.