What you need to know about Hyperthyroidism (Second part)
Today we continue with the second part of the hyperthyroidism discussion (first part here), talking about imaging studies and treatment

Imaging Studies
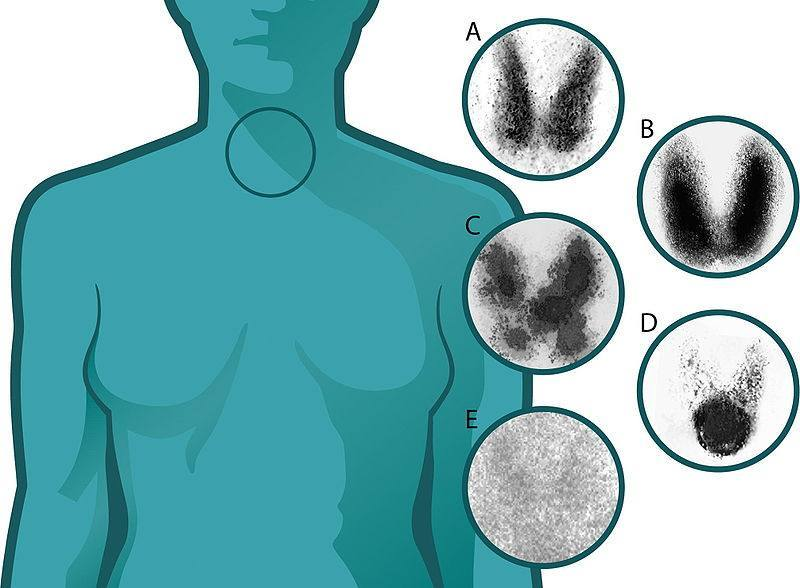
- Scintigraphy: it’s a test in which a contrast is injected that, in addition to giving an image of the thyroid, measures its capacity to store iodine. It can clarify what is the cause of thyrotoxicosis, since the pattern of uptake or storage changes according to the type of disorder:
-Graves-Basedow disease: a diffuse enlargement of the gland is evident, with uniform and elevated uptake of the radioactive iodine (B).
-Toxic multinodular goiter: irregularity would be evident, with relatively diminished uptake areas and other areas of increased uptake. The total uptake would be slightly to moderately increased (C).
-Toxic adenoma: total uptake is normal and only one hypercaptant nodule is seen between the rest of the suppressed thyroid tissue (D).
-Subacute thyroiditis: a very low uptake of radioactive iodine would be evident (E).
- Thyroid ultrasound:
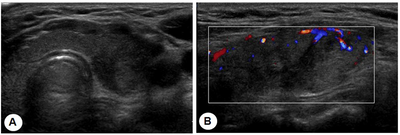
-Graves-Basedow disease: there is a diffuse enlargement of the gland, which is observed hypervascularized.
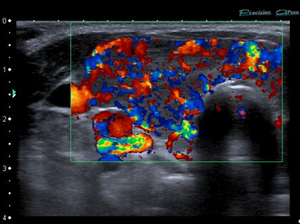
-Toxic multinodular goiter: there is also an increase in the size of the gland but with the presence of several hypervascularized solid nodules.
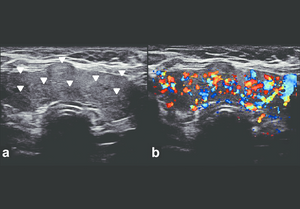
-Toxic adenoma: a normal-sized gland is usually found with a single hypervascularized solid nodule.
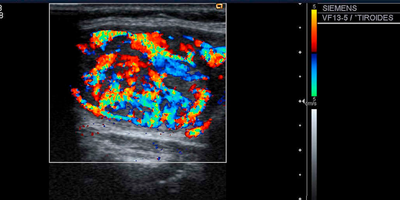
-Subacute thyroiditis: an enlarged gland can be seen, with areas with a tendency to form nodules but with decreased vascularization.
Treatment
It includes the relief of symptoms, treatment with antithyroid drugs, therapy with radioactive iodine-131 and surgery (thyroidectomy).
- Symptomatic treatment
-Use of beta-blocking drugs for the relief of tremors, nervousness, palpitations. The most used is Propanolol.
-In cases of mild ophthalmopathy use artificial tears and sunglasses. In more severe cases, steroids, ocular decompression surgery and ocular radiations are used.
- Antithyroid drugs
-These drugs block the production of thyroid hormones in the gland.
-The most commonly used are methimazole and propylthiouracil.
-They are not useful in the treatment of subacute thyroiditis (where the block is useless, since the previously formed hormone is already released).
-Useful for long-term control of hyperthyroidism in children and pregnant women. In adults, it is used to control hyperthyroidism until definitive therapy (radioactive iodine or surgery) is performed.
-The doses are adjusted every 4-6 weeks until the thyroid function normalizes.
-Some patients (20-30%) with Graves' disease experience remission of the disease after being treated for 12-18 months, although recurrences are common. In these cases of recurrences it is necessary to administer a definitive treatment (radioactive iodine or surgery). Patients with toxic multinodular goiter or toxic adenoma do not experience remission.
-Adverse effects: the most common are allergic reactions, however it may cause a decrease in the number of white blood cells, polyarthritis and hepatitis. Therefore, the patient must visit the endocrinologist every 3 months.
- Treatment with Radioactive Iodine-131
-Therapy of choice for hyperthyroidism.
-Thyroid hormones are made from iodine, therefore, the cells of the gland will take any form of iodine, radioactive or not.
-It is administered orally (in liquid or capsule).

-It causes fibrosis and destruction of the cells of the gland (no other organ or tissue will uptake the radioactive iodine).
-The response may take weeks to months.
-Adverse effects: in most cases the patient will develop hypothyroidism after treatment.
-Contraindicated in pregnancy, lactation and children younger than five years.
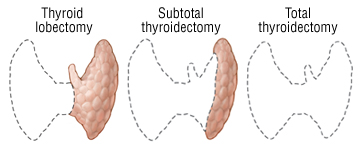
- Surgery (Thyroidectomy)
-It consists of the partial or complete removal of the thyroid.
-Preferably in pregnant women with intolerance to antithyroid drugs, in patients with large goiter and in patients with severe ophthalmopathy.
-Before performing the surgery, the patient must be controlled with antithyroid drugs.
-The patient subsequently develops hypothyroidism.
-Adverse effects: in addition to the risks inherent to surgery, there is a risk of damage to the recurrent laryngeal nerve and damage to the parathyroid glands, but these complications are rare.
I hope the information has been useful, until next post
Reference: