What you need to know about Hyperthyroidism (First part)
In this post I want to talk about another frequent disease in the endocrinology clinic: Hyperthyroidism.
I would like to start by differentiating two terms, that, although similar, do not mean the same, they are: thyrotoxicosis and hyperthyroidism.
The term hyperthyroidism is reserved for the condition in which the thyroid gland produces an excessive amount of thyroid hormone (overactive thyroid), instead, we refer to thyrotoxicosis when we talk about any condition in which there is an increase in amount of thyroid hormone in blood, that is, it includes all the conditions that cause hyperthyroidism and other entities (such as subacute thyroiditis or the administration of high doses of thyroid hormone, where there is no hyperactivity of the gland).
Causes
The main causes of thyrotoxicosis are:
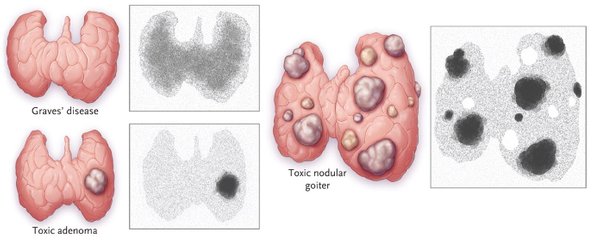
Graves-Basedow disease: it’s the most common cause, since it represents 60-80% of all cases. It’s an autoimmune disease where the presence of an autoantibody against the thyroid stimulating hormone (TSH) receptor causes a constant stimulation of the gland, which increases in size and produces more hormones. It is common between 20 and 40 years and like almost all thyroid diseases is much more frequent in women and there is a certain genetic predisposition.
Subacute thyroiditis: represents approximately 15-20% of cases. In this entity what happens is a destruction of the gland with release of the thyroid hormone previously formed and stored.
Toxic multinodular goiter: also represents 15-20% of cases. There are multiple nodules that produce a lot of thyroid hormones (hyperfunctioning).
Toxic adenoma: there is a single hyperfunctioning thyroid nodule. It represents approximately 3-5% of cases.
Treatment with high doses of thyroid hormone.
Induced by iodine: occurs in patients who ingest an excessive amount of iodine (to perform an imaging study with a contrast material, for example).
Struma ovarii: a type of ovarian tumor that contains ectopic thyroid tissue.
Patients with choriocarcinoma or hydatidiform mole in whom excessively high levels of human chorionic gonadotropin can activate the thyroid stimulating hormone (TSH) receptor.
Symptoms and signs
Among the most common signs and symptoms we have:
- Anxiety, nervousness, irritability (could be cases of psychosis).
- Heat intolerance.
- Weight loss.
- Hyperactivity.
- Insomnia.
- Increase in the frequency of evacuations.
- Muscular weakness.
- Brittle nails and hair.

- Tachycardia and cardiac arrhythmias.
- Hypertension.
- Wet and warm skin.
- Hands tremor.
- Decreased menstrual bleeding or less frequent menstrual periods.
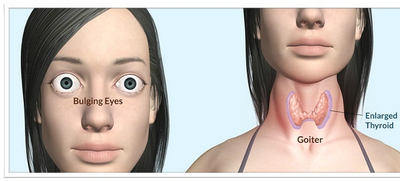
- Diffuse goiter (in the case of Graves-Basedow disease) or multinodular. If the goiter is large, it can cause compressive symptoms such as difficulty breathing or swallowing. It can also cause hoarseness (dysphonia).
- Ophthalmopathy: present in Graves-Basedow disease. There may be inflammation, tearing, shrinking of the eyelids, swelling around the eyes, bulging eyes (exophthalmos).
- Dermopathy: Also present in some patients with Graves-Basedow disease. There is thickening of the skin and edema. Common in pretibial regions.
- It can get to a very serious condition called thyroid storm, which requires admission to an intensive care unit.
Young patients tend to have more symptoms such as anxiety, hyperactivity, tremor and in older patients cardiovascular symptoms dominate.
Similarly, patients with Graves-Basedow disease tend to have much more marked symptoms.
Diagnosis
The diagnosis is confirmed mainly through the determination of the values of TSH (which will be low or what endocrinologist call suppressed) and of T3 and free T4 (which will be high).
Regarding antiantibodies, the following should be determined:
Anti-thyroid peroxidase or anti-TPO antibodies: although their elevation is not specific, they are positive in a high percentage of patients with Graves-Basedow disease.
Thyroid-stimulating antibodies or also known as anti-TSH receptor antibodies: positive in 63-81% of patients with Graves-Basedow disease.
This is all for today, very soon I will be publishing the second part (Imaging Studies
and Treatment).
Reference: