Joint prosthesis infections - JPI

Introduction
The increase in the placement of joint prostheses (hip, knee, shoulder, elbow, wrist, etc.) has led to an increase in infections associated with this surgery.
Early and accurate diagnosis is essential for greater success in treatment. The multidisciplinary approach by a team made up of traumatologists, infectious specialists, microbiologists specializing in joint prosthesis infections, radiologists, rehabilitators and specialists in Nuclear Medicine facilitates rapid diagnosis and allows the optimal treatment to be established from the outset.
Infection related to joint replacements is now a major public health problem in most developed countries. The practice of arthroplasty has been one of the most significant health advances in recent decades. The technological development, the progressive ageing of the population and the prolongation of the life of patients with underlying pathology have led to an exponential increase in the number of patients undergoing this practice.


Pathology of the infection in joint prosthesis
The particular characteristics of these infections are determined by the presence of the prosthetic biomaterial and its interrelation with host tissues and infecting microorganisms. The implant facilitates infection, which can occur with a very low bacterial inoculum (less than 100 colony forming units/g) and by low virulent and usually contaminating microorganisms. This predisposition varies according to the composition and properties of the biomaterial. The process of bacterial adhesion to the prosthesis and the subsequent formation of biolayers, in which the bacteria are agglutinated by a bacterial polysaccharide called slime. In the deepest biofilms the bacteria are in "dormant or stationary" phase, in a medium with low oxygenation, high amount of waste materials and low pH. These bacteria express a phenotypic antibiotic tolerance, with an increase in the minimum bactericidal concentration of the antibiotics.
75% of the cases are caused by Gram-positive cocci, with a high prevalence of staphylococci; 25% are S. aureus sensitive or resistant to methicillin and 35% are Staphylococcus coagulase-negative. Gram-negative bacilli, enterobacteria and Pseudomonas aeruginosa cause 10-15% of cases. In recent years, infections due to various species of Streptococcus and Enterococcus faecalis (10-15%) and among anaerobic bacteria Propionibacterium acnes (>5%) have been described more frequently. More than 10% are polymicrobial infections and in 10-15% of cases the cultures are negative.

Treatment
In a great majority of prosthetic infections a combined medical-surgical treatment with debridement or removal of the prosthesis and antibiotic therapy is required to achieve the eradication of the infection. The early treatment is a decisive element in the possibility of saving the arthroplasty.
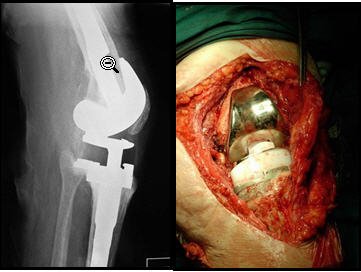
It is reasonable to initially consider debridement with retention of the prosthesis, if it is not loosened, the soft tissues are in conditions, we have effective antibiotics for responsible microbiology and the clinical picture does not exceed 3 weeks of evolution. Thus, the probability of curing these infections without removing the prosthesis is fundamentally related to the time of evolution of the infection and, therefore, to the degree of development of the bacterial biofilms, which "age" rapidly and become refractory to antibiotic therapy. Some doctors use a somewhat longer post-surgical period, 2 or 3 months, to define the bacterial population but the need for early treatment seems more appropriate. Some patients with infection are diagnosed beyond one month after surgery. In fact, it is often difficult to determine the time of clinical evolution, as the onset of pain or the appearance of problems in the surgical wound may not be evident. The cure rates with this surgical practice have been lower in retrospective series, but higher in prospective series, with optimal use of antibiotic therapy. The type of surgical debridement is decisive in the possibilities of curing the infection without removing the prosthesis and must be exhaustive and include the change of polyethylene, so that all the articular nooks and crannies can be accessed. In cases of uncemented prostheses, the surgical procedure can be used to temporarily remove the prosthetic components, extend the debridement and re-implant them again after sterilization.
Dr. Leopoldo Maizo - Orthopedic Surgeon


Firma diseñada por @themonkeyzuelans, contáctalos vía Discord "themonkeyzuelans#9087"
Great projects from the Steemit community:
- My Fundition campaign: https://fundition.io/#!/@drmaizo/6f88ggj8h


.png)
saludos dr, te escribo desde aca desde Caracas, para hacerte una consulta via discord
Hola @nahupuku, por supuesto, casi no tengo activado discord, me puedes escribir por instagram @drmaizo directamente y con gusto de ayudaré.
Ah vale, perfecto. Muchas gracias!
This project is being supported by @Fundition the next-generation, decentralized, peer-to-peer crowdfunding and collaboration platform, built on the Steem blockchain.
Read the full details of Fundition Fund program
Learn more about Fundition by reading our purplepaper
Join a community with heart based giving at its core
Fundition is a non profit project, by supporting it with delegation you are supporting 200+ projects.
50SP100SP200SP500SP1000SP2000SP5000SP10000SP