Drug-delivering Cells A Reality: Artificial Cells To Target Tumors And Deliver Drugs (Research-based)
While we are healthy, we pay less attention to our immune system, forgetting that our good state of health is because white blood cells are waging a steady war against invading bacteria viruses and parasites, tracking them down and eliminating them through a variety of mechanisms. Naturally, we continue in this attitude of being less concern about our immune system until such a time it is weakened, and we come down with a cold or flu. Of course, any defense can be overwhelmed. And hence our immune system is no exception.
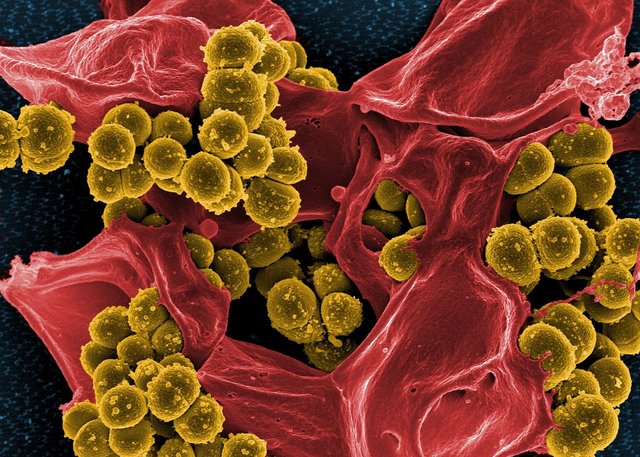
[Source: Pixabay CC0 licensed]
This explains why there has been increased research interests in this regards as researchers try to improve on nature through technologically creating their own white blood cells that are capable of exhibiting such evolutionary bequeathed characteristics of living cells as replication, compartmentalization, metabolism, movement, communication and environmental sensing and subsequent response. [1] Although research into this field is still at its infancy, substantial successes have been recorded by a number of scientists.
...the greatest potential applications lie in the realm of therapeutics: for responsive in vivo drug synthesis, engineered communication with diseased cells, hosting genes for gene therapy, and delivery of therapeutic enzymes, peptides and transplant cells. Source
Artificial cells and their mechanisms of drug delivery
Among the known scientists who have been making efforts to create man-made white blood cells that are capable of delivering therapeutic enzymes to targeted defective tissues, is a professor of chemical engineering and biological engineering at the University of Pennsylvania, known as Daniel Hammer.
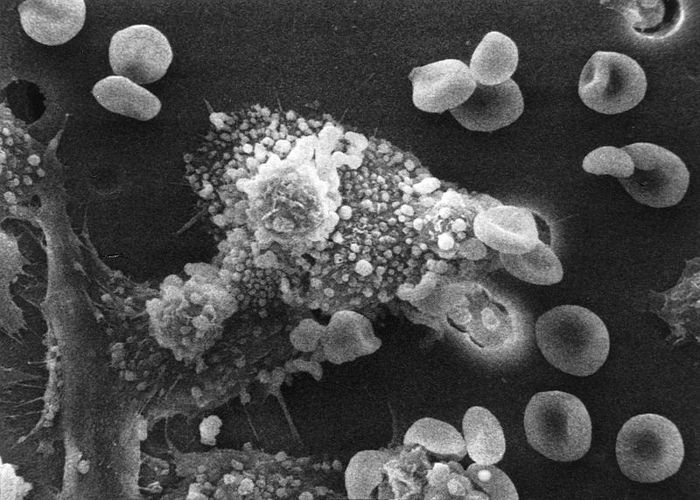
[Cancer immunology: in the diagram, Macrophage have identified a cancer cell (the large, spiky mass). Upon fusing with the cancer cell, the macrophages (smaller white cells) inject toxins that kill the tumor cell. [4]. Source: Wikimedia commons. Author: Susan Arnold. Public domain licensed]
For more than a decade, Professor Hammer studied how he could use plastics to create cellular structures that could mimic targeting capabilities and adhesive properties of white blood cells. The aforementioned traits allow white blood cells to not only take the fight to viruses and bacteria (in what Hammer described as molecular zip-coding) but also stand firm on ground to fight them.
...Think of a gel capsule of your preferred headache medicine but on a much smaller scale and with a programmable molecular brain...Source
For many years, Hammer's postulate remained in the realm of hypothesis as all attempts to validate it were to no avail. However, he remained unshaken in his belief that his concept of synthetic cells known as leuko-polymersomes could one day deliver the latest cancer-killing drugs directly to a tumor or send out a chemical beacon that signals natural white blood cells to come and join the fight against a disease. [2]
Working in collaboration with colleagues from Duke University, in 2010, Hammer successfully designed synthetic molecules that mimic the structures which enable white blood cells to locate and attach to defective tissues. These artificially produced molecules otherwise known as synthetic cells were later observed (in vitro) to find inflamed tissues and adhere to them.
[Illustration of drug delivery of the PEG-CPT NRs. Source: Wikimedia commons. Author: Fuqiang Guo et al. CC By 4.0 licensed]
Further experiments conducted by Hammer's team in collaboration with researchers from the University of Delaware showed that when shone with a blast of UV-light, the synthetic cells did not only find and attach to the inflamed tissues but also unravel and release their contents which could be therapeutic enzymes. That's an early step toward synthetic cells that could be programmed to release their contents on cue. [3].
Conclusion
Although Daniel Hammer is the world's recognized pioneer in the artificial cell-aided drug delivery, he is not the only one working in the endeavor as of today. There is a virus-motivated model currently being pursued by Tim Deming and his team at University of California, Los Angeles.
"If you view a virus as a very efficient delivery vehicle, that's what we're trying to replicate," Deming says.
Even at that, Hammer's model seems to be the best choice as our body still regard viruses as foreign agents and will always develop its own mechanisms to fight them. However, Daming and his team are currently working on how to overcome this pitfall. With successful perfection and standardization of synthetic white blood cells enabled drug delivery device, cancer afflictions and terminal diseases will be more effectively contained via precise delivery of appropriate therapeutics. Thanks for reading.
References for further reading
- Leuko-polymersomes
- Artificial cells: from basic science to application
- Vesicle-based artificial cells: recent developments and prospects for drug delivery
- Lab-created cells could target Tumors and deliver drugs
Yours truly,
@eurogeeFollow @eurogee, the Steemit's Witness Voting Advocate & Host, Show Us Your Witnesses Weekly Contest. Follow @euronation, An International Support Scheme For New And Struggling Steemians Join us on Telegram and whatsaap through the below links:
https://t.me/joinchat/HsUnkBJ083m0R6xIp4iA-A https://chat.whatsapp.com/9VhuK6475477fD7fPIYJ6i 
Don't Exit Without Voting For Witnesses! No Witnesses = No Steem Blockchain; If You Truly Love Here, Vote For Witnesses NOW! Click This Link To Vote Now Witnesses are equivalent to life and blood of steem blockchain. Without them, the blockchain will seize to function and we will all be stranded here. Click here to read more on why it is important to vote for witnesses

this is good stuff,.. Resteemed
@eurogee You have earned a random upvote from @botreporter because this post did not use any bidbots.