Blood Transfusion, or not?

Author: Three-shots, CCO Creative CommonsSource: Pixabay
We know now that they have fangs, are immortal until a protagonist manages to drive a stake through their heart, feed on blood, and many are aristocrats. As the vampire folklore expanded over the years and the stories about them garnered more characters, critics and drew the interest of many, their supposed characteristics and powers have undergone several amendments. But one thing remains constant- their mode of feeding.
They feed on blood. By sinking their supposedly sharp fangs into the neck of their victims. Be it fact or fiction, humans have long since regarded blood as sacred, a life source vital to human survival. And for good reason too. But it goes beyond a ‘super acknowledgment’ sometimes. It is almost worshipful, the regard for blood.
For the life of a creature is in the blood, and I have given it to you to make atonement for yourselves on the altar; it is the blood that makes atonement for one’s life.
Leviticus 17:11
In paganism, the ‘life-giving power’ of blood was regarded as an important ingredient in sacrifices and rites. Christians and Jews believed human blood has so much power it could atone for ‘sins’ and cleanse the soul off blemishes. Christianity and Islam have culturized this belief based on the command in the Bible and Quran not to eat meat which still contained blood.
Jehovah’s Witnesses, in particular, are known for their stance on blood transfusion, choosing obedience to the commandment on blood found in the Bible over their own lives.
It seemed good to the Holy Spirit and to us not to burden you with anything beyond the following requirements:
29 You are to abstain from food sacrificed to idols, from blood, from the meat of strangled animals and from sexual immorality. You will do well to avoid these things. FAREWELL
Blood transfusion is one of the breakthroughs in medicine that followed William Harvey’s work in physiology. Undoubtedly, it has saved lives. Is there any basis to the sociocultural and religious views regarding blood?
What is Blood Transfusion?
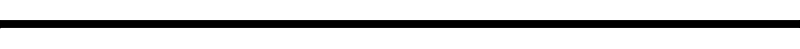
Blood transfusion is the process whereby blood or blood products are infused into a person intravenously following blood loss from accidents, diseases or surgery.
Blood transfusions are now so commonplace that they are a routine part of medical practice. They are so safe and life-saving that it is downright strange to refuse one when it’s needed.
With advances in medicine and increased awareness, the problem of donor blood availability and infections have been on the decline. Yet, blood conservation methods are important to limit an over-dependence on blood transfusions.
Blausen.com staff, (2014), WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436 CC BY 3.0, from Wikimedia Commons
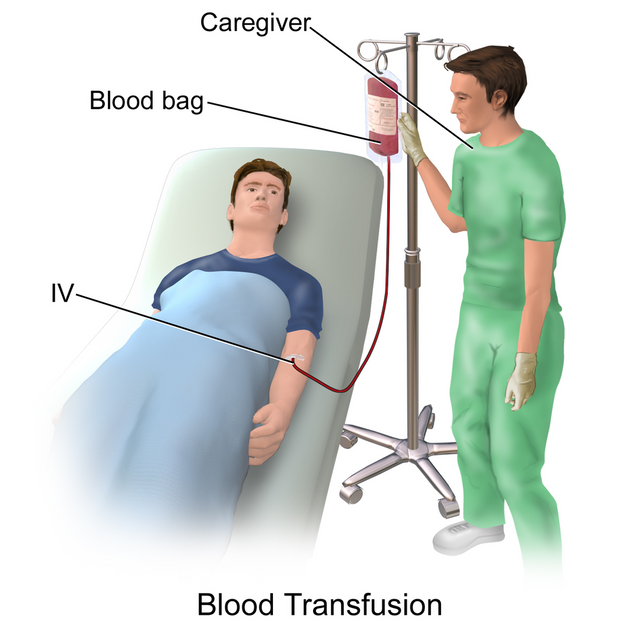
Like most medical research, blood transfusion research began with transfusions between animals in the 17th century. Researchers attempted the same experiment, transfusing animal blood into humans with fatal results. The most hilarious and morbid example is that of Pope Innocent VIII who was opportune and unfortunate to be the recipient of the first blood transfusion. His personal Physician at the time, Giacomo di San Genesio, gave him the blood of three 10-year-old boys to drink. The similarity between this ‘blood transfusion’ and the blood drinking vampires might put a question mark on the fictionality of vampirism. The sacrificial boys later died. Although there’s no credence to this story, it is almost logical to imagine the earliest form of blood transfusion would have occurred this way. The first successful blood transfusion was from a sheep to a fifteen-year-old boy, done by Dr. Jean-Baptiste Denys. It is difficult to understand how the boy survived. Maybe the volume of blood transfused was small enough that he withstood the allergic reaction or more improbably, he survived by blind luck. But his ‘luck’ ran out on his fourth and fifth patients who died following the animal blood to human transfusion. Blood transfusion with the use of blood typing only began in the 20th century. With the science of blood typing, a crude form of cross-matching was introduced as donor blood and recipient blood would be mixed before the blood transfusion. Dr. James Blundell in 1818 performed the first successful human blood transfusion. Despite this breakthrough, the probability of dying from a blood transfusion remained high. It wasn’t until 1901 when the human blood groups were discovered by Karl Landsteiner that blood transfusion became a science rather than a basketballer practicing his hoops. It is estimated that 85 million units of red blood cells are used in blood transfusions yearly. Despite its fatalistic history, blood transfusions have become of the most common procedures in medicine. The blood used for blood transfusions can come from two sources. People who experience any of the following may need a blood transfusion. Blood comes with a ‘label’ and is grouped according to this labeling assigned by specific antigens on the surface of red blood cells. There are thirty-five such groupings of blood but the most important two are the ABO and RhD antigens. Special immunoglobulin proteins called antibodies recognize and is specific to each antigen. The antigens and antibodies of the ABO system are: For the Rh system, the most important antigen is the D antigen. To reduce the risk of a transfusion reaction following a blood transfusion, the donor’s blood and the recipient’s blood are cross-matched for agglutination both visibly and microscopically. If agglutination occurs, the blood will not be transfused to the patient. Author: JuralMin, CCO Creative CommonsSource: Pixabay People who have been exposed to Variant Creutzfeldt-Jakob disease (vCJD) are not eligible donors because of the risk of transfer through a blood transfusion. Failure of cross-matching will lead to a hemolytic reaction. Where the antibody destroys the foreign red blood cells. Blood can be transfused whole or in parts depending on the patient’s needs. Jehovah’s Witnesses reject blood transfusions in whole or in part on religious grounds. For this reason, they make use of various alternatives to whole and fractionated blood rather than ‘break their faith.’ Apart from Jehovah’s witnesses, some patients might prefer the use of ‘blood substitutes’ to blood transfusion. With advances in medicine, bloodless surgeries are becoming more successful. Regardless of the advancements and successes, bloodless surgeries and the use of alternatives to blood transfusions comes with its own risks. Some Jehovah’s Witnesses have died due to their objections to blood transfusions. Jehovah’s witnesses are not forced by the organization to object to blood transfusions but their stance has contributed to an increased use of alternatives. Rather than go straight for the blood transfusion option, health practitioners check out the alternatives either for economic reasons, blood scarcity or the patient’s preference. These alternatives serve different goals to either expand blood volume or enhance the oxygen-carrying capacity of the blood. However, they are no viable alternatives to adequately enhance oxygen carrying capacity in event of severe blood loss. Yet. Some of the alternatives used are: In their efforts to boost athletic performance, athletes have been to known to boost their blood volume through intravenous blood infusions to improve their cardiovascular function and oxygen delivery to starving muscles. No doubt, blood transfusion has evolved into a life saving medical procedure. At least, you must be thankful you don't need to take in blood by drinking. In the future, even more effective alternatives might be made available to those with special preferences. I guess this is where free will comes in. We have a choice, we have hope and we have our lives. As humans, we are under obligation to respect others and the choices they make. Yet, within those choices must come knowledge, perseverance and hope so we can always make informed decisions. Blood
Moral, sociocultural concerns and alarm over the increasing fatalities led to the ban of blood transfusion for the next 150 years.Prevalence
Paradoxically, the number of blood transfusions performed yearly is on the decline and predicted to decrease even further as advances in medicine and blood conservation is reducing the need for it.Blood transfusion procedure
Who needs a blood transfusion?
ABO Blood groups
Even after cross-matching, the blood is further screened for the presence of infectious agents like bacteria, HIV, hepatitis B, and C,
Other adverse effects like anaphylactic reactions, fever, post-transfusion purpura, and infections may follow inefficient cross matching.Types of blood transfusions
Blood doping
Athletes do this through blood transfusions and the use of synthetic erythropoietin to enhance red blood cell production.References
Blood doping
Blood transfusion
Vampire
Leviticus
William Harvey
How long does a blood transfusion last?
Jehovah’s witnesses and Blood transfusions
Quality Alternatives to blood transfusion
Blood Substitute and Erythropoietin Therapy in a Severely Injured Jehovah's Witness
Blood substitute
Blood type
Hi @vanessahampton I am not sure why the emphasis on Jehovah’s Witness in this article?
Was there? I think it's almost impossible to discuss blood transfusion without discussing their stand on it. I hope I was objective, or i tried to be.
Hello! I find your post valuable for the wafrica community! Thanks for the great post! @wafrica is now following you! ALWAYs follow @wafrica and use the wafrica tag!
Congratulations! Your post has been selected as a daily Steemit truffle! It is listed on rank 7 of all contributions awarded today. You can find the TOP DAILY TRUFFLE PICKS HERE.
I upvoted your contribution because to my mind your post is at least 30 SBD worth and should receive 139 votes. It's now up to the lovely Steemit community to make this come true.
I am
TrufflePig, an Artificial Intelligence Bot that helps minnows and content curators using Machine Learning. If you are curious how I select content, you can find an explanation here!Have a nice day and sincerely yours,
TrufflePig