Bleeding and How it Stops; Bleeding Disorders
Bleeding is something everyone has experienced at some point in their lives, some people less frequently than others. Bleeding results from a damage to the walls of blood vessels (arteries and veins) leading to the leakage of blood outside the blood vessels. For bleeding to stop, clotting or coagulation has to take place. This involves a number of factors to be realized. Certain blood cells (platelets), clotting factors, vitamins (particularly K) as well as blood vessels (arteries and veins) play individual roles in bleeding as well as clotting.
HOW BLEEDING IS STOPPED (Hemostasis/Blood Clotting/Coagulation)
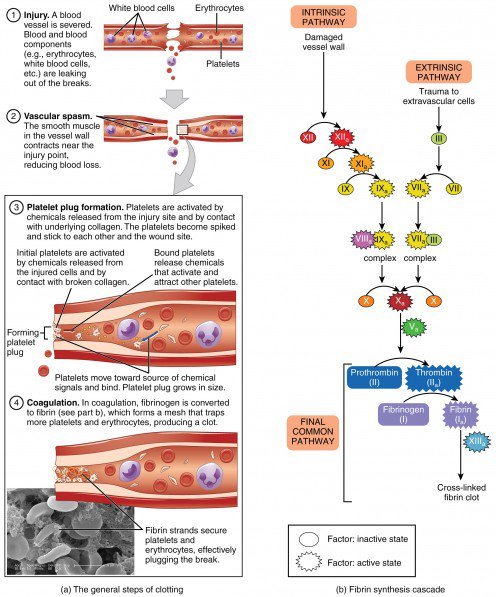
Hemostasis is a complex process that has a lot of steps but for the sake of simplicity, the steps are grouped into three (3).
Vasoconstriction
Blood vessels contain elastic fibres in their walls which give them the ability to expand or narrow depending on the need. Therefore vasoconstriction is basically the narrowing of blood vessels in this case as a response to bleeding. As the blood vessels narrow, the amount of blood lost is minimized. This has its own limitation as blood vessels cannot completely become shut through their own constrictive ability in response to bleeding. This is where the next stage comes in.
Platelets Activation and Aggregation
Platelets are small cells in the blood produced during the process of red blood cells development. In response to bleeding, these platelets become activated. They get attracted to each other at the site of bleeding. They stick together to form a temporary plug at the site (of damage of blood vessel) thereby temporarily stopping blood loss. They release chemicals that bring other platelets to the site and also cause further narrowing of the blood vessel.
Formation of Blood Clot
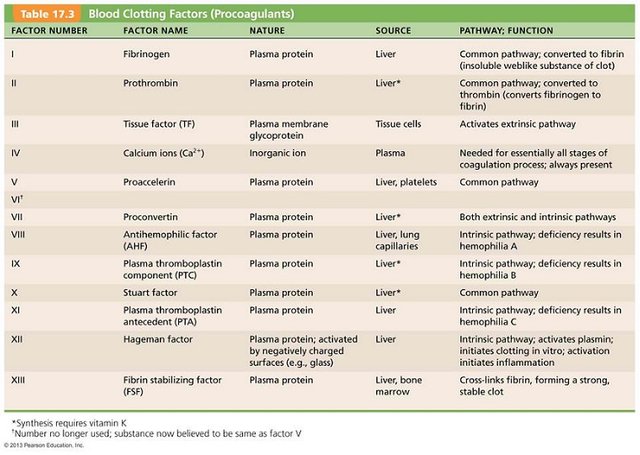
This is a complex process with its function being to reinforce the platelet plug with fibrin fibres to give it a longer-lasting effect. There are two (2) pathways (Extrinsic and Intrinsic) through which blood coagulation/formation of blood clot happens. However, both lead to a Common Pathway.
The extrinsic pathway is initiated by the action of a Tissue Factor released by damaged cells at the injured site. It is named the extrinsic pathway because it is initiated by cells outside the blood vessels. Intrinsic pathway however is initiated when blood comes in contact with collagen fibres within torn wall of blood vessels which is why it is called intrinsic.
The two pathways ultimately lead to the production of Prothrombin Activator which in torn triggers the Common Pathway. Here, the Prothrombin activator triggers Prothrombin which is turned into Thrombin. Thrombin then acts as an enzyme to convert Fibrinogen to strands of Fibrin. The fibrin fibres/strands hold the damaged vessel walls together until the wound heals. It is then broken down in a process known as Fibrinolysis.
COMMON BLEEDING DISORDERS
Depending on whether the clotting factors in the blood are absent or blood vessel abnormality is involved, different bleeding disorders would be noticed.
HEMOPHILIA
This is an inherited disorder. It is an X-linked recessive disease that causes absence of two main factors in the clotting cascade- factor VIII (For Hemophilia A) and factor IX (Hemophilia B). It is most commonly seen in males. It's incidence is about 1 in 5000 live births for hemophilia A and 1 in 30000 live births for Hemophilia B. Due to the absence of these factors, blood clotting cannot be achieved hence prolonged bleeding.
People with this disorder usually have prolonged bleeding into joints (ankles are most common bleeding sites in children), muscles, gastrointestinal mucosa, and sometimes bleeding into the brain.
Treatment involves preventive measures and clotting factor replacement.
- Patients are advised to avoid contact sports; helmets, knee and elbow pads are recommended when doing activities that leave those areas prone to bruising or injury.
- Immediate medical help is very important once bleeding is noticed.
- Factor VIII and IX replacement with doses given as required.
von WILLEBRAND DISEASE
This is also a genetic disorder where there is a defective or absent von Willebrand Factor (vWF- a protein involved in the clotting cascade). This disrupts the clotting cascade. According to statistics, it is the most common bleeding disorder.
Symptoms include: frequent nose bleeds, easy bruising, bleeding excessively after a procedure like tooth extraction or surgery.
There are three (3) major types of von Willebrand disease (vWD) and a fourth known as Acquired von Willebrand Disease. Types 1 and 3 are seen in people with quantitative vWF deficiency; symptoms are usually mild and severe respectively. Type 2 is seen in individuals with qualitative deficiency. In type 2, the symptoms are mild to moderate. Acquired vWD results from an autoimmune disease like Lupus or some type of cancer as well as being induced by certain medications.
Treatment is mainly with Desmopressin Acetate (it's a synthetic version of the hormone- vasopressin). It stimulates the release of vWF from cells.
VASCULITIS
This is the inflammation of blood vessels. When blood vessels are inflammed, they are susceptible to damage leading to bleeding. A good example is Henoch Schoñlein Purpura. It is an autoimmune disease characterized by the inflammation of small vessels all over the body with majority of symptoms seen in the skin, joints, gastrointestinal tract and kidneys.
Symptoms include
- Rash (95-100% of cases)
- Abdominal pain
- Hematemesis (Bloody vomiting)
- Joint pain and swelling (especially the knees and ankles)
- Bloody stools.
- Bleeding into the brain can present with stroke-like symptoms
Treatments are mostly supportive. However analgesics (ibuprofen, Naproxen) and Corticosteroids are used. Cytotoxic drugs like Azathioprine, Cyclophosphamide are used in some cases.
Other bleeding disorders - Idiopathic Thrombocytopenic Purpura, Immune Thrombocytopenic Purpura, Thrombotic Thrombocytopenic Purpura, Disseminated Intravascular Coagulation.
Bleeding disorders can also. E triggered or caused by other primary diseases. Examples are Leukemia, infection/sepsis, Liver disease. Liver disease in particular is a major culprit due to that fact that it is responsible for the production of most of the clotting factors in the blood. Liver failure leads to a corresponding failure of production of clotting factors.
The Hallmark of managing bleeding disorders is Preventing bruising/ bleeding and immediate medical help once symptoms are noticed.
THANKS FOR READING
DON'T FORGET TO UPVOTE, COMMENT, RESTEEM AND FOLLOW FOR MORE.
References:
American Society of Hematology
Medscape
National Hemophilia Foundation
Cleveland Clinic
Owlcation
Wikipedia
Epocrates



well done
Thanks