The biology and physics of wound healing (part 1 - the cellular players and dynamics of healing)
I thought that it will also be a cool idea to share glimpse of my research. I don't exactly work on wound healing, but I work on mechanisms that are required for proper healing of any tissue. More specifically, on the diseases that occur when these mechanisms fail. I will come to that, in time. Nevertheless, for today let's discuss the basics of how wounds heal. What are different processes and phases that work together to seal a cut?
Image by Ulleo | CC0
Alright then, let's talk about wound healing. But, let's first talk about the tissue on which you witness wounds quite frequently. A place where you can watch them heal. An organ your are most familiar with - the skin.
The skin and its residents
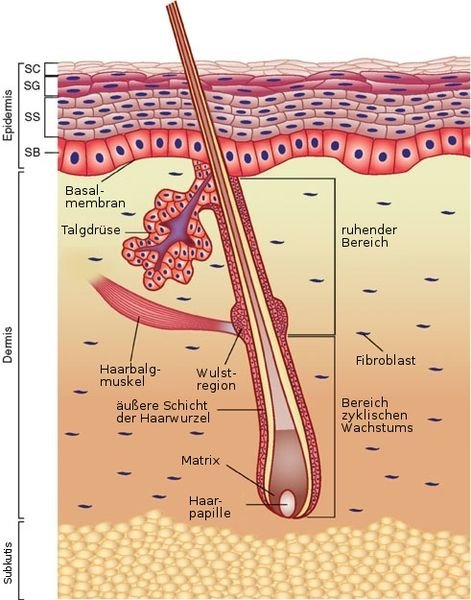
*Image from Wong, D.J. and Chang, H.Y. Skin tissue engineering (March 31, 2009), StemBook, ed. The Stem Cell Research Community, StemBook, doi/10.3824/stembook.1.44.1. Derivative work: Anka Friedrich. | CC BY 3.0 *
Wounds can occur and heal in any organ. But, skin is my favorite organ to understand the healing process. For starters, it's easily accessible to naked eye. Also, getting a piece of skin and looking at it under a microscope is a pretty easy task. And once you have knowledge of the basic mechanics of healing in skin you can just extrapolate and compare this knowledge to what happens in other organs. So what is this organ made of? What are the different parts of this organ? And what cells live in which part?
You can divide the skin into two main compartments. The epidermis and the dermis. The epidermis is what you see with your naked eye. Well, the dead layer of it to be precise. Below, this dead layer (stratum corneum) of cells, lies the live and kicking layers of epithelial cells(keratinocytes). The bottom most layer lives on this thick deposition of protein matrix called the basement membrane. This stratum basale layer is undifferentiated, and contains the precursor stem cells, which will progressively diffrenriate into a next layer (stratum spinosum) and then the next (stratum granulosum), until they finally become cornified, dead and visible to your eyes.
Below the basement membrane is territory of different kind of cells. It's a jungle of collagen and other extra cellular matrix proteins. In this jungle, reside these cells called fibroblasts. If you think of the extra cellular matrix as cement, that holds the tissue together; the fibroblasts are maintenance workers, that produce this matrix and also maintains its organization.
There are of course other compartments in the skin. Right below the dermis, there is hypodermis, which contains the fat cells. The dermis also contains the blood vessels and the nerves. There are immune cells that reside in the dermis. There are melanocytes at at epidermal-dermal junction, which gives you, your skin colour. There is arrector pili muscle that gives you those goose bumps. Then there are hair follicles, sweat glands and sebaceous gland. We may revisit these other things if need be. For now I just want you to remember the epidermis, the basement membrane ,the dermis, epithelial cells, and fibroblasts along with the matrix they make and maintain. That should do for now.
The dynamics of wound healing.
Image by Häggström, Mikael (2014). "Medical gallery of Mikael Häggström 2014". WikiJournal of Medicine 1 (2). | Public Domain
So, what exactly happens right after you get the cut? Which cells are recruited at what time? And, more importantly, how each of these cell types, contribute to the healing process?
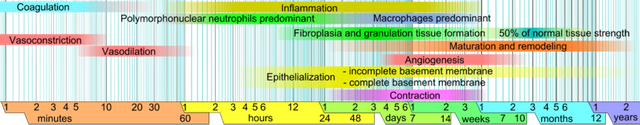
Hemostasis - Just seconds after the cut
As soon as there is a cut on the skin, your cells must sense it and recruit the repair guys. The cells in the epidermis are held together tightly by adherns junctions. There is certain amount of tension in the sheet of cells. So as soon as you make the cut, the sudden release of tension, alerts them. Same holds for the damaged blood vessels. The damage cells also release damage associated molecular patterns or DAMPs. The non damaged cells in response to the mechanical cue and DAMPs secretes the factors that starts the healing process. Other processes also include calcium flux and hydrogen peroxide response of cells in the wound environment (Niethammer, 2016).
Vasoconstriction
The first and foremost response other than pain (that makes you withdraw from source of injury) is body trying to minimize the blood loss. The blood vessels constricts, reducing the blood flow to the wound.
Clotting
Also in attempt to minimize the blood loss, the platlets release the clotting factors, in response to injury. The role of platelets is not only limited to clotting but in the clot, they also secrete a matrix of protein called, Fibrin. This will act as temporary matrix over which keratinocytes can move and fibroblast can migrate to. The platlets also secrete many growth factors and cytokines to induce the neighbourhood to start would healing response (Laurens et al., 2006).
Inflammation - from few minutes to few days
Vasodilation
Once the blood loss has been minimized next task is to clear off the debris and prevent infections. For immune cells to be recruited, the blood vessels need to dialate again. It starts about 5 - 10 minutes after the wound and lasts for hours. The blood flow peaks at the wound site and remains elevated for days (Rendell et al., 1997).
Inflammation
The wound proximal epithelial cells, fibroblasts, platlets, and blood vessels send signals for immune cells to be recruited. The first responders are cells of innate immune system - neutrophils, soon followed by macrophages. While the main purpose of neutrophils is to clear off bacteria and debris, they also cause some collateral damage. They secrete proteases enzymes and other proteins that are packed in their granules to kill off any nearby cell. While that may at first, look unnecessary, but it can be argued as an important defense mechanism. Just to be sure that any unwanted, infected and exposed cell does not remain in vicinity (Wang, 2018). The macrophages on the other hand are like these janitors who have multiple jobs at their hand. One, which is obviously to clear off any debris, just like neutrophils. Second, they also stick out there through out the entire process where they secrete signals to - attract other immune cells, promote blood vessel formation, cause proliferation of fibroblasts, and also help in remodeling the matrix along with fibroblasts after the wound is healed (Adamson, 2009, Rodero and Khosrotehrani, 2010.
Even the resident immune cells such as gamma-delta T cells aka dendretic T cells which live in epidermis and dermis get activated. Their major role, apart from secreting anti-microbial peptides is to help with growth of keratinocytes and re-epithelialization of the wound (Jameson et al., 2002.).
However, I don't want you to underestimate the resident epithelial cells, when it comes to keep off the microbes. They are the first layer of defense, and they know very well that those opportunistic pilifucker bacteria that live on skin and in air, are not going to miss the party. So, while they send the signals for recruitment of immune cells, they secrete these proteins called antimicrobial peptides. So if the microbes were invaders, and immune cells are solders, then anti microbial peptides are like landmines (Braff et al., 2005).
The conventional cells of adaptive immune system, lymphocytes - Helper and cytotoxic T cells, come in later. Together they clean up the mess in the wound and keep it infection free. The helper T cell and cytotoxic T cells are however known to slow down healing and bit. Plus they are also implicated in scar formation, since the mice lacking lymphocytes shows starless wound healing (Boyce et al., 2000, Gawronska-Kozak B et al., 2006).
The inflammatory phase lasts for about 4-6 days. After which most of the immune cells gets deactivated or die via apoptosis. The T-regulatory cells are recruited and activated at this stage to overlook the supervise this demise of inflammation (Nosbaum et al., 2016).
Proliferation and sealing the skin
While, immune cells are doing their job the resident cells needs to restore the tissue architecture. But first they need to make up for the cells that have been lost. So all the nearby stem cell niches in epidermis and in hair follicles are woken up. There is a massive expansion of undifferentiated layer of keratinocytes. Same is true for the fibroblasts in dermis as well. They expand in numbers and began their descent towards the site of injury (Pastar et al., 2014). This starts somewhere in day 2 - day 3.
Re-epitheliazation
The sheet of these expanded undifferentiated epithelial cells, move in top of the new matrix layed down in dermis. The process continues until they cover the entire wound (Geer et al., 2003, Pastar et al., 2014). The covered area also starts to simulatenously differntiate to form the other layers.
Fibroblasts - the construction workers at work.
While a temporary matrix is layed down by fibrin secreted by platelets, to restore the original tissue you need the cells that makes the native matrix. So resident fibroblasts, along with other cells that diffrentiatiate into fibroblasts start to accumulate in temporary matrix. Here they proliferate and secrete extra cellular matrix proteins such as collagen and fibronectin. This matrix replaces the temporary matrix and makes environment favorable for blood vessels and nerves to repopulate (Brainbridge, 2013).
The contraction phase
However, there is something else the construction workers do, in order to accelerate the healing process. While secreting the collagen matrix they also start expressing alpha smooth muscle actin (a protein usually found in smooth muscle that helps them contract). They hold tightly to collagen matrix and contract, pulling the would edges together (Berry et al., 1998).
Remodelling phase
Even though now completely sealed and closed, it is important to restore the tissue architecture to normal state. They process begins after contraction and continue for years to come. In this process the activated fibroblast either mellowdown or die via apoptosis. The remaining fibroblasts continue to secrete metaloproteases and their inhibitors regulating the mechanical properties of matrix they deposited. The idea is to get the matrix charactertics back to how it was before the wounds. How efficient this remodelling process is also marks a distinction between a repair that ends up in a scar vs a total regeneration of the organ (Li and Wang et al., 2009, Atala et al., 2011).
I guess that's enough wound healing for the day. In future articles I will go into depth of discussing, how perturbation of these different phases in wound healing are Hallmarks of different diseases. Specifically, overscarring fibrotic diseases and cancer.
About steemstem
But before I go I would like to mention about the steemstem platform. Well, if you love reading and writing interesting science articles @steemstem is a community on steem that support authors and content creators in STEM field. If you wish to support steemstem do see the links below.
You can vote for steemstem witness here -
Quick link for voting for the SteemSTEM Witness(@stem.witness)
Delegation links for @steemstem
Quick delegation links: 50SP | 100SP | 500SP | 1000SP | 5000SP | 10000SP).
Delegating to @steemstem gives ROI of 65% of the curation rewards.
References
Niethammer P. The early wound signals. Curr Opin Genet Dev. 2016;40:17-22.
Rendell et al., 1997. The Skin Blood Flow Response in Wound Healing
Wang J. Neutrophils in tissue injury and repair. Cell Tissue Res. 2018;371(3):531-539.
Braff et al., 2005. Cutaneous Defense Mechanisms by Antimicrobial Peptides.
Signing off
@scienceblocks

This story was recommended by Steeve to its users and upvoted by one or more of them.
Check @steeveapp to learn more about Steeve, an AI-powered Steem interface.
Thankyou, Steve!
Interesting article.
Btw @scienceblocks : Someone I met at ACTREC was telling me that L'Oréal funds wound healing research(even at NCBS). Is it true? Or just rumor?
They do. A part of it, at least. There are other companies too. However, majority of it is still core funding.
okay
Hey scienceblocks,
very cool post. I also want to make something about it. This healing processes also covers a plethora of changes within the participating cells as well as in the entire body.
Veryi nteresting field.
Regards
Chapper
Indeed, there are a lot of changes. The field is too vast to be covered by any single post or a person. It would be nice to see your post on this. I would be eagerly waiting for it.
I do my best, but this year it probably won't work.
See ya next years
Cheers
Chapper
Ah, I miss medical school. Now I can barely remember regarding the subject. You did a great job! Is your research related to diabetes mellitus? I just figure since diabetics would have a slow healing process compared to healthy people.
Thanks. I did work on role of immune system in diabetes in a small project. And our lab does work on wound healing in diabetes as well. But my research is about pathology of fibrosis and tumor stroma.
This post has been voted on by the SteemSTEM curation team and voting trail in collaboration with @utopian-io and @curie.
If you appreciate the work we are doing then consider voting all three projects for witness by selecting stem.witness, utopian-io and curie!
For additional information please join us on the SteemSTEM discord and to get to know the rest of the community!
Hi @scienceblocks!
Your post was upvoted by Utopian.io in cooperation with @steemstem - supporting knowledge, innovation and technological advancement on the Steem Blockchain.
Contribute to Open Source with utopian.io
Learn how to contribute on our website and join the new open source economy.
Want to chat? Join the Utopian Community on Discord https://discord.gg/h52nFrV