Hyperosmolar hyperglycemic state: an acute complication of diabetes.[EN]
Hello Steemians this time I want to talk about one of the acute complications of Type 2 Diabetes Mellitus, and it is the hyperosmolar hyperglycemic state, before as known as " hyperglycemic hyperosmolar nonketotic coma ", the term "coma" was set aside since it really courses with varying degrees of altered consciousness and not always the patient is in a coma.
This complication occurs most of all in patients with diabetes mellitus type 2. It is typically that elderly patient with increased urine volume, weight loss and loss of appetite with few weeks of evolution and that eventually presents alterations of consciousness that can go from drowsiness to coma.
It can also occur in patients diagnosed with diabetes mellitus type 1 or a severe state of hyperglycemia (greater than 300 mg / dl).

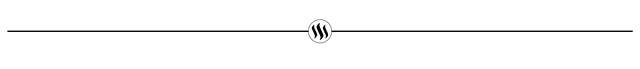
Stress: serious infections such as septicemia or pneumonia, surgery, burns, myocardial infarction, stroke, among others.
Effect of some drugs: drugs that favor hyperglycemic states such as steroids, beta-blockers, diuretics such as thiazides, furosemide (loop diuretic), minoxidil (direct vasodilator), diazoxide (very hyperglycemic).
Other: food transgression (mass consumption of carbohydrates), use of intravenous hypertonic solutions, lack of exercise.
Pathophysiology
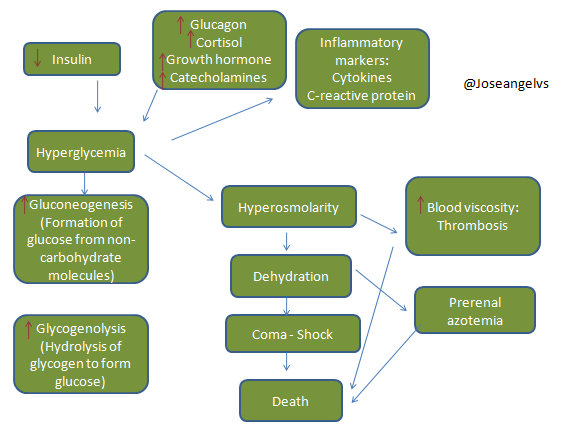
The mentioned causes condition to hyperglycemia, together with the relative deficit of insulin and the peripheral resistance to it, trigger a series of physiopathological events:
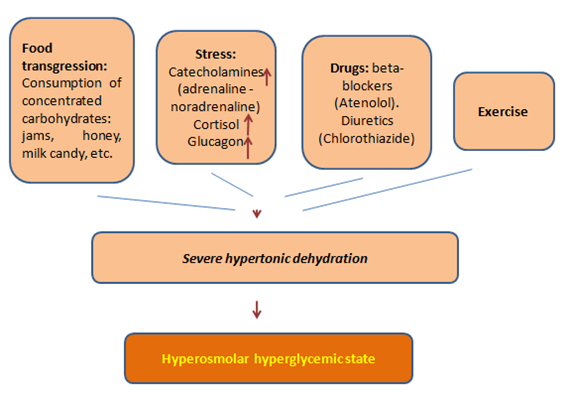
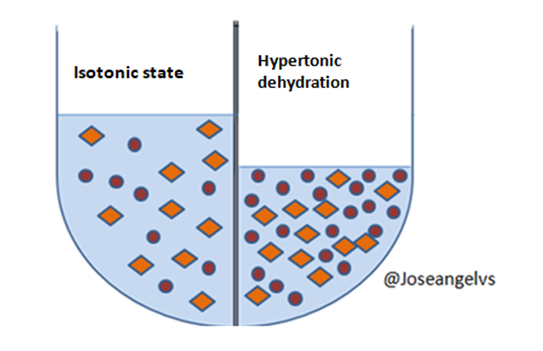
- Osmotic diuresis: When the level of glucose that is in the blood exceed 180 MG/dl, there is greater excretion of glucose in the urine (and less resorption) and glucose has osmotic activity which drags more water conditioning hypertonic dehydration (it refers that there is greater loss of water and not of salts) so the blood that is in the body is "more concentrated".
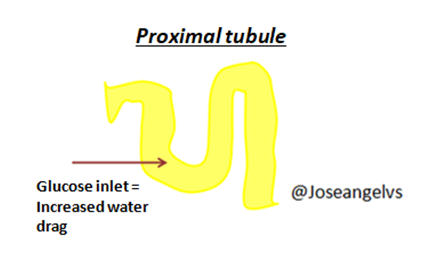
- In the hypothalamus there are receptors (osmoreceptors) capable of detecting minimal changes in blood osmolarity, stimulating the release of a hormone (vasopressin, synthesized in the hypothalamus and stored in neurohypophysis) stimulating thirst as a way to enter more water to the body and thus try to replace the lost water.
Insulin is a hormone that tells the body that there is an excess of glucose in the blood and tells the body to activate the mechanisms to save it (formation of liver and muscle glycogen) or store it in the form of fat. And there are the counterregulatory hormones that are those that rise when there is no insulin, indicating that energy is needed telling the body to take glucose out of its reserves (fat, muscle and glycogen).
This deficit of insulin coupled with the increase of counterregulatory hormones force the liver to increase glucose synthesis through the mechanisms of gluconeogenesis (synthesis of glucose from non-sugar macromolecules, such as amino acids or fats) and glycogenolysis (hydrolysis of glycogen stored to form glucose).
In addition the lack of insulin and the increase of hormones such as Glucagon generate an enzyme imbalance in the liver, disfavoring the enzymatic pathways for the generation of energy (ATP) from the oxidation of glucose and favoring the formation of more and more glucose.
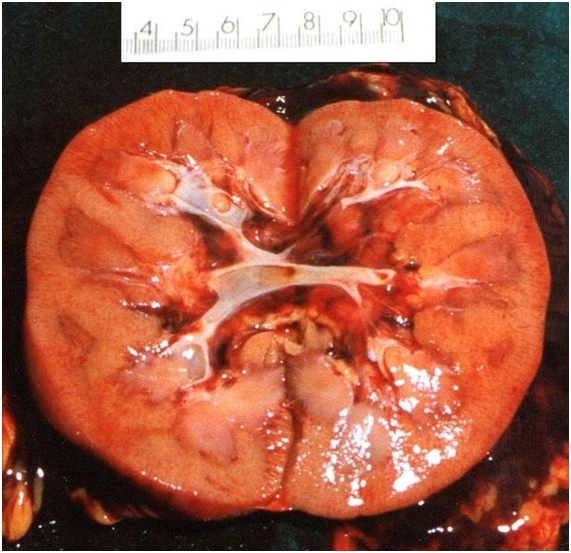
Dehydration can cause nitrogen retention (accumulation of waste substances in the blood) by decreasing blood flow to the kidney.
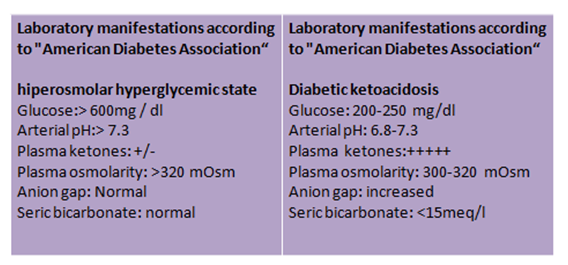
Diagnosis
To make the diagnosis you must first suspect it. It is more common in elderly people with type 2 diabetes but it must be remembered that this is not always the case, it can occur in type 1 diabetics or in other states of severe hyperglycemia.
The evolution of the disorder is slow, the patient reports an increase of thirst and increase of urinary volume. In the physical exploration we can find arterial hypotension, increase of the respiratory frequency, increase of the cardiac frequency, mucous membranes and dry skin, and affectation of the state of the conscience that can be variable until arriving to a comatose state.
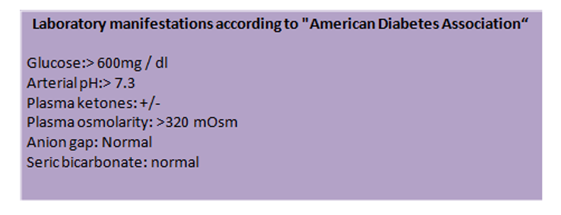
Differences with diabetic ketoacidosis
Diabetic ketoacidosis is another acute complication of diabetes, but in this case it is more common in type 1 diabetes.
In the diabetic ketoacidosis the evolution of the disease occurs more quickly, the patient reports weakness, increased thirst, increased urinary volume, abdominal pain and vomiting. In the physical exploration we found a deep and rapid breathing (Kussmaul breathing), a increase in the heart rate and signs of dehydration.
The treatment is based on 3 fundamental pillars:
Determine and treat the triggering cause.
Treat dehydration: The dehydration is long evolution so the hydrolytic restitution must be balanced, the first is to expand with saline solution to 0.9% (if the sodium in blood is more than 150 meq/Lt should be used hypotonic solution of 0.45%) in the first 3 hours. After this, indicate hypotonic solution at a rate of 200-300ml/hr for 2 or 3 days.
- Correction of hyperglycemia: Normally correcting dehydration decreases glycaemia but also should indicate a intravenous insulin regimen in two phases: first a bolus of 0.1 units / kg and then consistently 0.1 units / kg / hour. The administration of intravenous glucose should go hand to hand with the evaluation of blood glucose every hour.
In addition, arterial blood gases and serum electrolytes should be evaluated every 4 hours.
Bibliographic references
- Fauci AS, et al. Harrison’s principles of internal medicine. Vol 2. 19th ed. New York: McGraw Hill; 2015
- Ramirez J. Modulo endocrinologia, numero 6. editora medica colombiana S.A 2007.
- Penna S. Fisiopatologia del sistema endocrino.Primera edicion. Venezuela; 2006.
- Kitabchi AE, Umpierrez GE, Murphy MB, Barrett EJ, Kreisberg RA, Malone JI, et al. Management of hyperglycemic crises in patients with diabetes. Diabetes Care. Jan 2001;24(1):131-53.
- Kitabchi AE, Umpierrez GE, Murphy MB, Kreisberg RA. Hyperglycemic crises in adult patients with diabetes: a consensus statement from the American Diabetes Association. Diabetes Care. Dec 2006;29(12):2739-48.


Congratulations! This post has been upvoted from the communal account, @minnowsupport, by Joseangelvs from the Minnow Support Project. It's a witness project run by aggroed, ausbitbank, teamsteem, someguy123, neoxian, followbtcnews, and netuoso. The goal is to help Steemit grow by supporting Minnows. Please find us at the Peace, Abundance, and Liberty Network (PALnet) Discord Channel. It's a completely public and open space to all members of the Steemit community who voluntarily choose to be there.
If you would like to delegate to the Minnow Support Project you can do so by clicking on the following links: 50SP, 100SP, 250SP, 500SP, 1000SP, 5000SP.
Be sure to leave at least 50SP undelegated on your account.