The Blue Baby Syndrome (Part 1); Introduction To The Tetralogy of Fallot
Hi everyone,
I didn't have much free times for the past couple of weeks, but when I'm free, it is time to share something related to medicine. Today, we're going to talk about the Tetralogy of Fallot, a set of congenital heart defects which could cause serious complications without appropriate interventions. Some of you might have heard about the Blue Baby Syndrome before, and I must clarify, it does not specifically refer to the Tetralogy of Fallot. The Blue Baby Syndrome refers to any conditions usually related to heart or blood which could potentially lead to cyanosis, a condition whereby the skin or mucous membrane of an individual turns blue as a result of poor oxygen saturation or inability for the blood in the circulation to fulfill the body's demand for oxygen.
Cyanosis can simply be divided into two which are central and peripheral. In medical school, I was taught on how to check for either of these condition through a thorough physical examination. Peripheral cyanosis usually refers to any bluish discoloration of the distal compartment (hands or feet) and central cyanosis can usually be examined around the lips or tongue. Pretty simple right? Theoretically, yes, but clinically, patients might present with a different set of symptoms which could indicate they were in the state of hypoxia (reduced oxygen saturation in the blood); that's why clinical experience is of utmost importance in making an accurate clinical diagnosis.
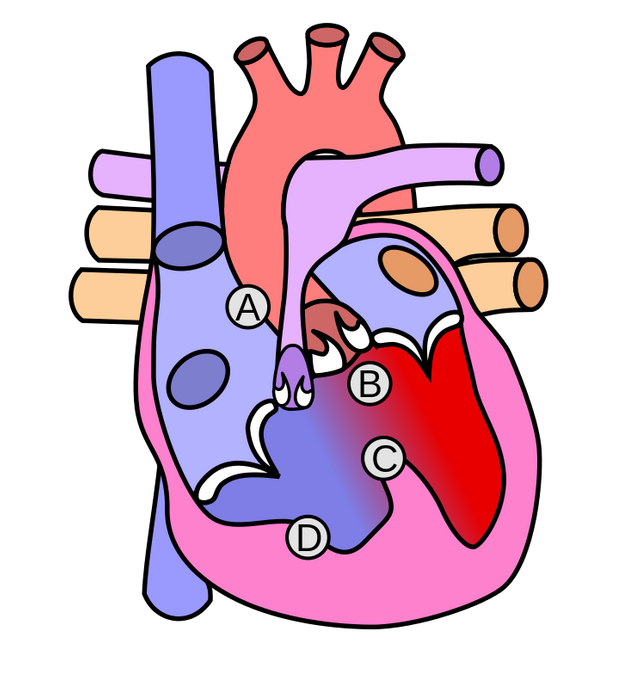
As the name indicates, the Tetralogy of Fallot (TOF) consists of 4 kinds of cardiac-related pathologies which are:
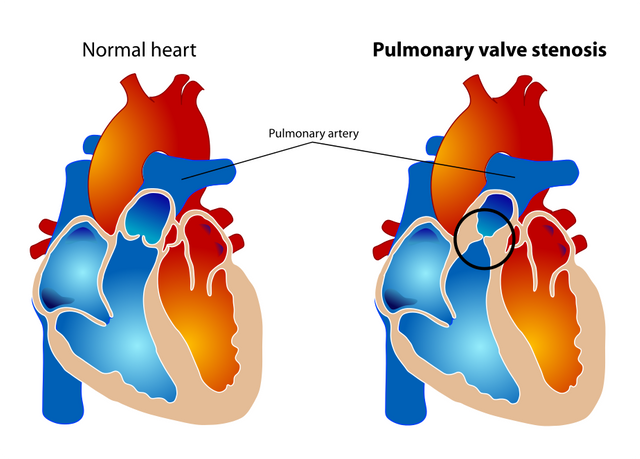
A) Subpulmonary stenosis
B) Overriding aorta
C) Ventricular septal defect (VSD)
D) Right ventricular hypertrophy
Even though this condition can lead to serious sequelae, the mortality rate of patients who were born with TOF is quite low. If you want to talk about the life expectancy of patients with TOF 30 years ago, most of them (approximately 85%) survived to their 40s; some even gave birth to a few babies which signifies that the medical care for this condition has been great since then. Nowadays, the field of medicine has advanced significantly compared to the last 30 years and the quality of life of individuals with cyanotic heart diseases have improved. This is attributable to the advanced of medical and surgical management which leads to a deeper understanding of the pathological aspect of diseases and its potential cure.
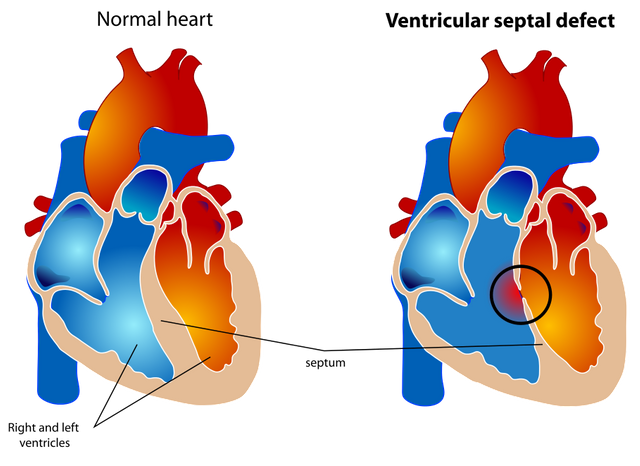
The ventricular septal defect
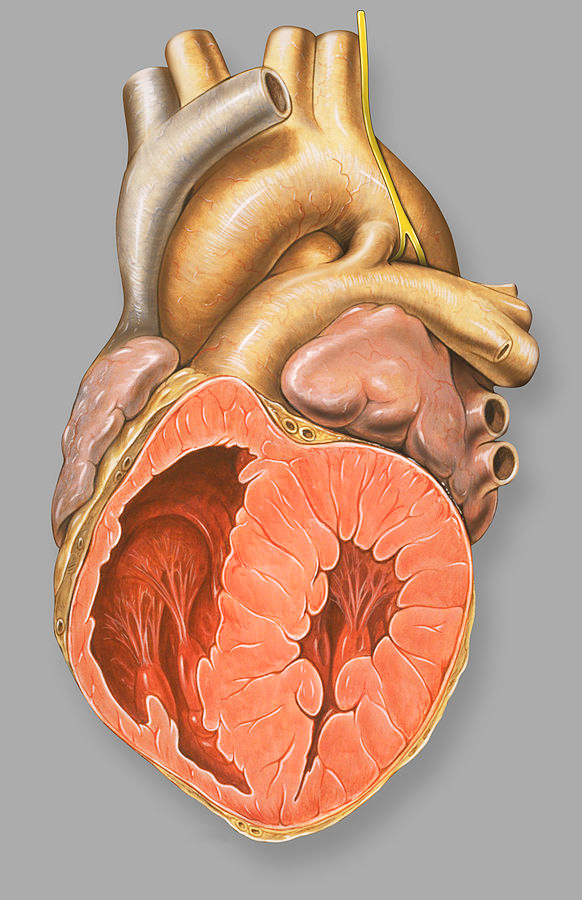
The ventricular septal defect (VSD) is a fancy term for a hole in the wall of the ventricle of the heart. I'm not going to outline the overall anatomy of the heart but what you need to know is, a heart is made up of 4 chambers. All of the chambers were working hard to pump blood either to the lungs to be reoxygenated or to the systemic circulation, supplying every single cell in the body with oxygen. Atria would serve as the entry point and ventricles as the resting chamber before the blood would be pumped out. Both of the atria would be separated by a muscular wall called the interatrial wall while ventricles would be separated from each other by the interventricular wall. I think by now you already knew that the ventricular septal defect describes a hole in the interventricular septum (wall).
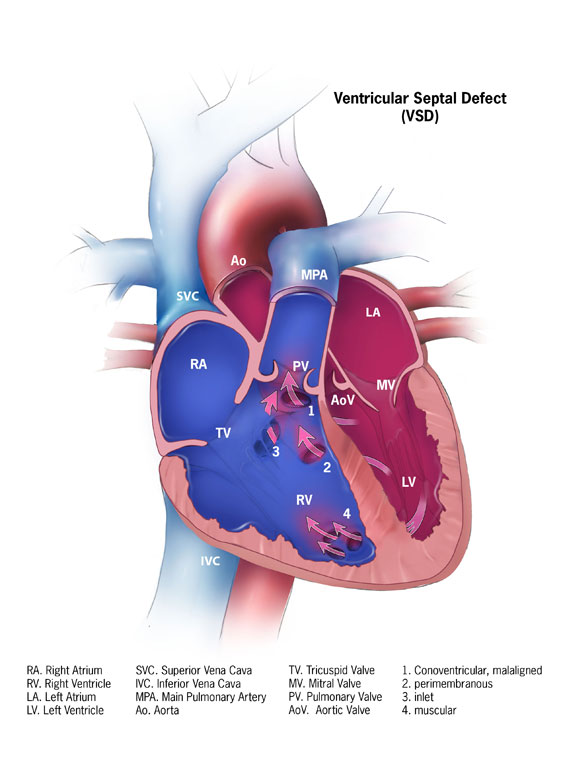
This hole will result in the mixing of blood from the systemic and pulmonary (related to lungs) circulation causing the oxygenated and deoxygenated blood to mix. As a result, the oxygenated blood portion which is pumped to the systemic circulation reduces making oxygen delivery less effective. There are two types of VSD which are:
- Muscular (affect the part of the ventricular wall which is filled with muscle)
- Perimembranous (affect the part of the ventricular wall which is adjacent to the tricuspid valve)
The severity of a VSD is often correlated to the size of the hole which caused blood to flow from the left chamber into the right chamber (due to the pressure difference). Either it is large or small would be determined by its size relative to the aortic opening. If the size of the interventricular septal is larger than the size of the aortic opening, then it is a large defect. Otherwise, it would be considered as a small defect. Patients with a small VSD were often asymptomatic, most of them only will become symptomatic if there are other external factors which affect their energy consumptions i.e. rigorous exercise, infection or pregnancy.
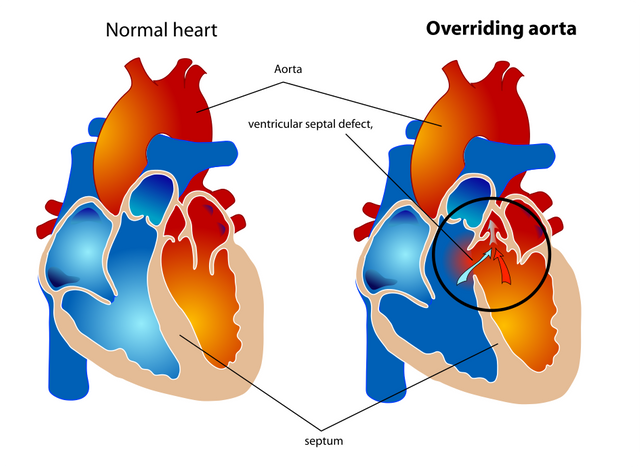
Overriding aorta, sub-pulmonary obstruction, and right ventricular hypertrophy
In a normal, healthy individual, the aorta would be the entry point of the oxygenated blood into the systemic circulation. In patients with TOF, the most common type of VSD would be the perimembranous type. A wall defect adjacent to the tricuspid valve provides an opening for the deoxygenated blood to pass through allowing them to be pumped into the systemic circulation. So why is it the blood from the right side of the heart can be pumped into the aorta considering the amount of pressure in the left side of the heart is higher than the right side of the heart?
This is because, in patients with TOF, they will also present with sub-pulmonary obstruction, which affects the pulmonary artery. All of the arteries in the body would carry oxygenated blood except for pulmonary artery; that was the rule of thumbs that have been taught in the medical school over and over again. The pulmonary artery will bring the deoxygenated blood into the pulmonary circulation to be oxygenated. The obstruction or narrowing was caused by various anatomical abnormalities in the trabeculae of the heart septum causing it to become narrow. This will lead to an accumulation of blood in the right ventricle caused by the obstruction hence, right ventricular hypertrophy (increased in size of the right ventricle).
As the volume increases, the pressure rises. This will cause the deoxygenated blood in the right ventricle to be "accidentally" pumped through the septal defect, into the aorta and finally, the systemic circulation.
The role of ductus arteriosus in the tetralogy of Fallot
Blaus - Wikimedia (CC BY 3.0)
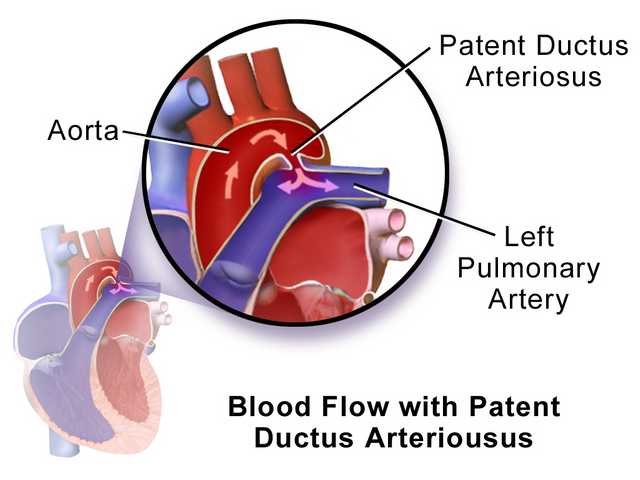
That's it, all of the components of the tetralogy have been explained. Most of the patients who were admitted to the hospital for TOF are neonates (between 0-28 days old) but then again it will depend on the severity of the defect. Some of the patients admitted to the hospital later when they were starting to show signs and symptoms of cyanosis associated with some respiratory distress. The reason why babies who were born were not hypoxic even with the heart defects is due to the fact that, there is a connection between the pulmonary artery and the proximal descending aorta. This connection was called ductus arteriosus.
Ductus arteriosus is a fetal blood vessel which will bypass the non-functioning fetal lungs to supply the other organs during infancy. In a normal individual, the ductus arteriosus will be completely closed after 2-3 days of life. It has to be closed to prevent blood flowing from the aorta into the pulmonary circulation causing signs and symptoms which resembles patients who were diagnosed with a VSD (It's a left to right shunt). There are two major factors which would cause the connection to close:
- Reduction of Prostaglandin E2
- Increase in blood oxygen concentration
If the connection persists, the condition is called a patent (or persistent) ductus arteriosus (PDA). In a normal individual, PDA can be thought of as a pathological process which can lead to heart failure but in a patient with TOF, PDA is a life savior. It provides an alternative route to the lungs so that the volume of deoxygenated blood being oxygenated can be optimized. It's a sophisticated mechanism which would allow the organs and heart to function at an optimum level. However, ductus arteriosus is just an alternative to alleviate the signs and symptoms before a much more definitive treatment (surgery) can be performed.
That concludes the first part of this series. In the next article, I will include a clinical case along with discussion regarding treatment modalities in treating TOF. If there is any mistakes or major grammatical error, please drop a comment. I'm in a hurry since night round would start in about 10 minutes or so. Thank you for your attention.
Sources
- Heart
- Blue baby syndrome
- Patent Ductus Arteriosus (PDA)
- Tetralogy of Fallot
- Tetralogy of Fallot: a morphometric and geometric study.
- Outcome after repair of tetralogy of Fallot in the first year of life
SteemSTEM is a community project with the goal to promote and support Science, Technology, Engineering and Mathematics on the Steem blockchain. If you wish to support the steemSTEM project you can:
Contribute STEM content using the #steemstem tag | Support steemstem authors | Join our curation trail | Visit our Discord community | Delegate SP to steemstem



Thanks for writing up an article to explain the famous tetralogy of fallot. very well written and easy to understand. The ductus arteriosus is thought to be a pathological connection actually plays a role in some congenital heart diseases in maintaining the oxygen supply in the blood stream.
Thanks for the feedback @soulesque. You were right, in some cases, PDA is an important vessel to keep someone alive. I would be writing about Transposition of Great Arteries (TGA) somewhere in the future.
Yeah TGA relies heavily on PDA. Without the connection, the baby is a goner. Thanks for the "refresher course" hahaha. I need it for the exams
Blue baby syndrome can also be caused by methemoglobinemia
Yes, you are right. 😉
Good job on getting SteemSTEM Distilled :)
Thanks @mathowl. I appreciate it. 😊
I agree with @soulesque: easy to understand. You manage to avoid technical terms, and when you use them, they're clearly defined. I stopped to read this because I remember my mother described one of my brothers shortly after birth as "turning blue". In his case it was transitory, but the condition that caused it was not. He had suffered irreversible brain damage. He dealt with that for the rest of his life.
I'm sorry to hear that @agmoore. Thank you for your feedback anyway.