Medical procedure "Paracentesis"
The following shared topic is very important in the medical area and is often practiced in the emergency services and especially gastroenterology is the evacuation of ascitic fluid through the abdominal wall, in order that this is diagnostic, ie to determine the etiology of this fluid or therapeutic in cases where the amount of intra-abdominal fluid is excessive, capable of generating pain and dyspnea, being necessary to evacuate it.
First of all we must consider that Ascites (also called Abdominal or Peritoneal Dropsy, Hydroperitoneum and Hydrops Abdominis) is defined as the abnormal accumulation of fluid in the abdominal cavity.
The term ascites derives from the Greek word askos, which refers to a bag or sac, the presence of which implies multiple pathologies that can trigger the presence of the same as is the case of liver cirrhosis generally associated with alcoholism and is responsible for 75% of the cases of ascites, then those of neoplastic origin in 10%, finally, heart failure in 5% and the remaining of varied etiology.
Peritoneal aspiration of ascitic fluid or paracentesis was first described by Solomon in the early 20th century. With the use of diuretic-type drugs, as well as the means of complications to this technique, paracentesis fell into disuse in the 1950s, being replaced by diuretic drugs, since the complications originated by this procedure were probably caused by the large caliber of the needles used to perform the drainage.
It was not until the end of the 1980s that studies and publications demonstrated that paracentesis was a safe and very useful procedure, and today this technique is common in the emergency department.

Public domain pixabay
Paracentesis is a very useful and important diagnostic tool, especially for those patients who have ascites again, that is to say, of new appearance, and with this end, a sample of said liquid is taken and the etiology of the same can be determined, as is the case with longstanding ascites, which over time generate a tense abdomen with a large amount of liquid inside, making it necessary to evacuate the same, improving the patient's breathing pattern and the level of comfort in these cases.
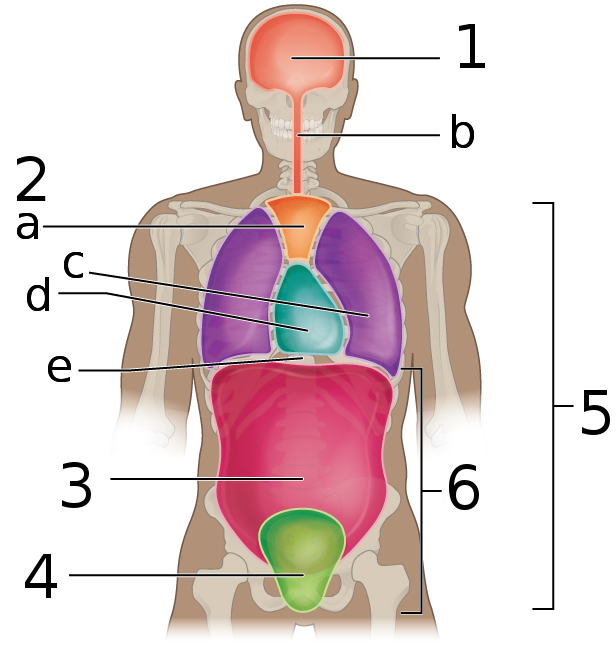
Anatomy
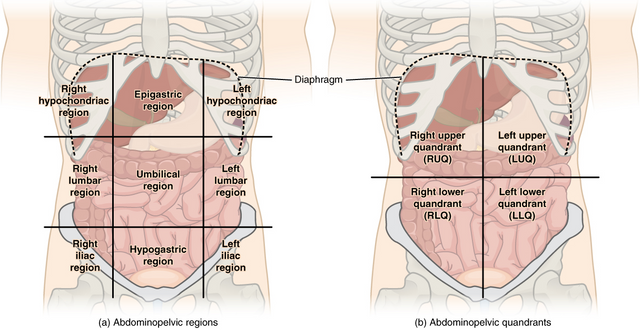
The general anatomy of the abdomen is well known to physicians and it is important to review it when performing a paracentesis.
The abdominal cavity is delimited by the peritoneum and protected from the outside by the musculature of the abdominal wall, adipose tissue and skin. The left and right rectus muscles, which are nourished by the epigastric vessels, are joined at the alba line in a totally avascular manner.
The navel is located along the lower portion of the linea alba. The layers of muscle structures in the anterior abdominal wall vary above and below the level of the anterior superior iliac spine.
The liver in conjunction with the gallbladder is located in the upper right quadrant, while the spleen is normally located in the upper left quadrant and when it increases in size by some process it can be felt in the lower ipsilateral quadrant.
The intestines occupy the majority of the abdominal cavity and are not attached, which allows their mobilization throughout this cavity.
The bladder is located in the pelvis, but can ascend to the abdominal cavity and is distended by urine.
The abdominal cavity is divided into compartments according to the mesenteric fixations. Ascitic fluid can be found anywhere in the cavity and this will depend on the amount of fluid and position of the patient, as the fluid follows the law of gravity and small amounts usually accumulate in the pouch, while large amounts can be found by bathing the intestines.
Indications
It can be run for both diagnostic and therapeutic reasons. A paracentesis or abdominal emptying is justified in a patient with de novo ascites, to establish the origin of the fluid.
When peritonitis is suspected to take cultures of the fluid, in those cases of patients with established liver disease who have tension ascites and need to evacuate it.
Paracentesis has been used to assist in the diagnosis of ruptured ectopic pregnancy, intestinal perforation and hemoperitoneum from abdominal trauma.
Public domain licensed CC BY 4.0)
Contraindications
There is no absolute contraindication to practicing paracentesis. Relative contraindications include patients who are pregnant or have an abdominal history, intestinal obstruction or coagulopathy.
Preparing the patient
The procedure, its risks and benefits should always be explained. Informed consent is obtained. The patient's bladder must be empty.
It is recommended that a nasogastric tube be placed prior to the procedure so that iatrogenic gastric perforation is less likely.
There are two recommended areas for paracentesis. The primary site is located in the midline and 2 cm below the umbilicus. As an alternative, the site 4cm to 5cm above and medial to the antero-superior iliac spine of the lower quadrants can be used. The lower left quadrant is preferred in order to avoid the spleen and sigmoid colon.
Care should be taken in regions with a scar, prominent veins, or an area of inflamed or infected skin to minimize complications.
The patient is placed in a right seated position for a midline approach or also called linea alba, in a right lateral position for a right lower quadrant approach, or in a left lateral position if a left lower quadrant approach is desired.
The patient is prepared. The skin around the desired puncture site is cleaned. Povidone-iodine solution is applied and allowed to dry. 2 ml to 5 ml of local anaesthetic solution is injected subcutaneously and along the path of needle insertion.
Techniques
Z-track technique
A Z-track is used to decrease the possibility of ascitic fluid leakage, especially in the case of stress ascites.
It is initiated by applying traction to the skin above or below the site of needle insertion, so that the skin is kept taut when the needle enters the peritoneum. The idea is that when the skin tension is released, the skin will return to its normal position and the paracentesis needle's path will be sealed.
An 18 gauge needle, a 14 mm needle and a 60 ml syringe are connected. Insert slowly and advance the needle perpendicular to the skin at about 45° and in the direction of the flow. Apply negative pressure with the syringe as you advance.
You should feel a loss of strength as the needle enters the peritoneal cavity. Needle advance stops when ascitic fluid enters the syringe.
The omentum or a loop of intestine can occlude the needle and thus the ascitic fluid can suddenly stop flowing in the syringe. The aspiration should be reattempted and if it fails it should be replaced.
The needle should never be placed while the tip is in the cavity, as this may lacerate the omentum, the bowel or a blood vessel. We proceed to remove the needle to the subcutaneous cellular tissue and then advance it again to the peritoneum.
The color, clarity and consistency of the extracted liquid is observed. About 30 to 50 ml are aspirated if the procedure is for diagnostic purposes, it is suggested to take samples for culture, cytological and cytochemical of the ascitic fluid.
If the reason for the paracentesis is for drainage, the needle is connected to an intravenous system, the flow end of which is connected to an aspiration bottle or bag to drain the necessary amount.
Finally, the needle is withdrawn in a Z-trajectory, so that the fluid does not leak into the skin, a dressing is applied to press the puncture site and compression is performed.
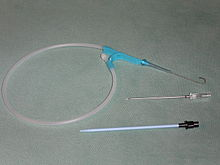
Seldinger technique
First described by Seldinger in 1953, this technique allows the placement of a catheter on a metal guide. The puncture site is chosen and the patient is prepared for the procedure.
The needle is inserted in a Z-travel while negative pressure is applied with the syringe. The entry of fluid into the mouth of the needle means that the tip of the needle is inside the peritoneal cavity. The needle is held firmly and the syringe is withdrawn.
The mouth of the needle is covered with a sterile gloved finger, this will provide air in and liquid out. Insert the metal guide through the mouth and advance the needle to the desired depth.
Hold the guide firmly in place, and pull the needle out over the guide. A small notch is made in the patient's skin adjacent to the guide with a scalpel needle. The cutting edge of the scalpel blade is directed away from the guide to avoid cutting it.
The dilator is passed through the sheath to form a unit, the dilator and the sheath are advanced over the guide, and the progress continues.
Advance the sheath until the catheter mouth is against the skin, hold it firmly, and remove the guide and dilator as a unit. A syringe is connected to the catheter and suctioned to confirm the intraperitoneal situation.
Finally, the catheter is clamped, the syringe is attached and the end is attached to an intravenous system connected to an aspiration bottle or drainage bag.
The catheter is removed once the procedure is complete and a dressing is applied to the puncture site.
Complications
They are rare, but they have been described and evidenced. Common ones include abdominal wall hematoma, hemoperitoneum, intestinal perforation, persistent ascitic fluid leakage and systemic hemodynamic involvement.
Intestinal perforation during paracentesis is rare and most of these lesions seal spontaneously and do not generate subsequent problems. Other complications such as generalized peritonitis and wall abscesses have also been reported.
In those cases where ascites fluid continues to flow through the abdominal wall, suturing the puncture site simply solves the problem.
Another more frequent complication observed after rapid removal of ascitic fluid is hemodynamic compromise, as removal of large quantities may trigger hypovolaemia significant, which must be corrected immediately.
Analysis of the ascitic fluid
Normal ascitic fluid appears yellow. Increased turbidity may suggest infection, elevated triglyceride levels, or other causes. Bloody fluid is common in neoplastic processes, intraperitoneal bleeding from intra-abdominal organs (from iatrogenic or spontaneous causes), or tuberculous peritonitis.
Specific analytical tests for the fluid should reflect the suspected diagnosis, such as simple fluid analysis with differential cell re-encounter, cultures and albumin concentration are all that is needed in uncomplicated liver cirrhosis.
Peritoneal carcinomatosis should be suspected and cytology requested, and even more so in those patients with a history of cancer. Mycobacterial cultures have a sensitivity of 50% and should be requested when tuberculous peritonitis is suspected. All potentially infected ascitic fluid should be cultured by direct inoculation into culture bottles.
Paracentesis is a common procedure in emergency medicine practice, there are few contraindications for it and it is mainly performed for diagnostic purposes to determine the presence of spontaneous bacterial peritonitis, as well as for therapeutic purposes in cases of stress ascites.

steemSTEM is a project of the chain of blocks that supports the scientific content in different areas of science. If you want to know more about this wonderful project you can join the server in discord
This article will be published at https://www.steemstem.io/
link
If you have any questions about any topic of medicine or present any disease you can comment the publication or write me in discord and I will attend you.
Dr. Ana EstradaI hope you enjoyed my content.

Hello @anaestrada12,
Your article caught my eye because I've had some experience with ascites. The first time I experienced this, a rather ignorant and ill-mannered physician suggested I was an alcoholic. The next time I had it, the doctors suspected obstruction or vasculitis.
Happily, on both occasions the event was acute, sudden onset, and resolved spontaneously. CT scans were a big help in getting to an underlying cause. I would think this would be the first step in any attempt to diagnose and treat. While the pain is significant in a patient with acute ascites, CT scans help to clear up the picture. Though paracentesis is relatively safe, still there is risk. (I am never eager to have someone stick a large needle in any part of my body haha)
The CT scans were extremely helpful afterwards, as doctors tried to assess what was causing these acute episodes. We--they and I--wanted to understand how to prevent future episodes and also to understand how to proceed safely if these occurred again.
I know your blogs are written for practitioners, but I hope you know that patients are also your readers. As a patient, I view my role in any treatment plan as collaborative. The doctor may know more, but well-written articles (such as yours) help patients to take an active role in formulating treatment plans.
Thank you for this information. Very valuable to all.
Greetings @agmoore2 thanks for the article, every patient is different, every pathology is different, and not all behaviors are the same, and of course every study that is requested has its indications in your case that only tomographic studies were necessary.
:)
Yes, I was lucky. I had excellent medical care (mostly) before, during and after my episodes. Very grateful for that.
@tipu curate
Upvoted 👌 (Mana: 20/30 - need recharge?)
Thank you @tipu
Thank you very much @girolamomarotta :)
🙏
This publication has been manually curated by the Steemitas Club Team. Thanks @anaestrada12 for sharing us this great post.
Steemitas Club is a community who give free delegations of 100 SP to new steemians and also has a curation project to support original content.
Thank you very much for the support @steemitasclub
This post has been voted on by the SteemSTEM curation team and voting trail. It is elligible for support from @curie and @minnowbooster.
If you appreciate the work we are doing, then consider supporting our witness @stem.witness. Additional witness support to the curie witness would be appreciated as well.
For additional information please join us on the SteemSTEM discord and to get to know the rest of the community!
Thanks for having used the steemstem.io app and included @steemstem in the list of beneficiaries of this post. This granted you a stronger support from SteemSTEM.
Thanks to the best blockchain community for all the support given in my two years in steem :) @steemstem
According to the Bible, Graven Images: Should You Worship These According to the Bible?
Watch the Video below to know the Answer...
(Sorry for sending this comment. We are not looking for our self profit, our intentions is to preach the words of God in any means possible.)
Comment what you understand of our Youtube Video to receive our full votes. We have 30,000 #SteemPower. It's our little way to Thank you, our beloved friend.
Check our Discord Chat
Join our Official Community: https://steemit.com/created/hive-182074