After 1, 2, 3, & 4 shots of vaccines, you can still get covid. So what will make people realise that vaccines don’t work?
I am posting this with the expression permission of Duncan Buckley. The original post is on Quora.
It is best to draw the distinction here and clarify that we now live in a world where the definition of “vaccine” and the understanding of what constitutes one has been altered.
Traditional vaccines use inert, weakened parts of the target antigen to help the body recognise the virus and mount an immune response upon the possibility of infection.
modRNA gene based therapies are not traditional vaccines, even though they have been pitched to this bracket of medicinal product (mainly to avoid the tighter regulations on gene therapy). The concept hinges on the utilisation of the recipients cells to internally manufacture the target part of the antigen to generate the immune response before those cells that get transfected by the instructions are destroyed.
Now, to return to your question, let’s analyse it objectively. If the modRNA injections “actually worked” as advertised, after two “primary series” shots, the body would have learned the formula for responding to the SARS-CoV-2 virus and be able to create cross reactive antibodies to deal with any mutated variant from the original WH1 strain (as our bodies have been doing naturally for centuries). Being a respiratory virus, much like influenza across the years, mutations happen.
Has that cross reactivity happened? Did people that had those original shots not get breakthrough infections? No.
“Oh but that’s the point! The injections don’t prevent infection they just reduce your chances of severe infection. As the virus mutated, it was necessary to keep the antibodies high to fight it”
But antibodies are no measure of neutralization capability. Even the FDA knows and advised that.
Many of the answers you’ve already received from the pro-modRNA crowd are adamant that no protection should be derived from infection, “because that’s not how vaccines work”, yet they miraculously protect the recipient from severe illness. Logically, if a person has a severe enough viral load to cause viremia, then no mechanism exists to protect from severe infection that may lead to hospitalization or death.
Equally that’s not how the virus works either.
Every iteration of a virus mutation lends towards a lesser virulent strain, so repeated injections using outdated strain configurations don’t help. The injections don’t train the immune system to prevent infection, the virus variant escapes the Wuhan configured antibodies, and so cannot impact the severity of disease. They needed less shots, not more of the same configuration that didn’t exist against differing variants.
But let’s look at the mechanisms - The one area that the pro-advocates like to avoid in favor of either loosely defined criteria, retrospective observational studies, or computational models that don’t contain real people.
It is already established fact that the modRNA injections encode for only single one part of the virus: the spike protein. Before the bivalent shots were attempted, the only target protein was in the configuration of the original 2020 strain from Wuhan (with some conformational changes). These same shots continued right through all the variants prior to and including Omicron emergence.
How was it known that prior to the modRNA shots in 2021, antibodies wouldn’t neutralise the virus when targeting the Receptor Binding Domain of the S protein? This, from 2014:

We conclude that using either single nAbs or dual nAb combinations to target a SARS-CoV RBD epitope that shows plasticity may have limitations for preventing neutralization escape during in vivo immunotherapy.
We found that neither single nAbs nor two nAbs in combination blocked escape. Our results suggest that targeting conserved regions with less plasticity and more structural constraint rather than the SARS-CoV RBD-like region(s) should have broader utility for antibody-based immunotherapy.
Breakthrough infections began almost immediately in March 2021[1] during the Alpha variant.
What should have been widely communicated was the calculated infection fatality rate[2][3] (IFR based on laboratory confirmed seroprevalence) for many demographics, but considering that was dutifully ignored to keep the fear of the virus high into “plague” levels of consciousness, use of the more mailable case fatality rate (CFR) was used instead.
Then there are those that advocate having “5 shots and it’s not hurt me”. Repetitive shots of lipid nanoparticle modRNA? There’s research about that too.
- Extended immunizations impaired the serum neutralization activity
- Extended immunizations suppressed the formation of germinal center
- Extended immunizations inhibited the activation of CD8+T cells
And the kids? What has this insane drive to “inject kids to protect granny” from a virus that doesn’t harm that age group?
At V2 + 28, interferon-γ and monocyte chemoattractant protein-1 responses to S. aureus, E. coli, L. monocytogenes, BCG vaccine, H. influenzae, hepatitis B antigen, poly(I:C) and R848 stimulations were decreased compared to pre-vaccination. For most of these heterologous stimulants, IL-6, IL-15 and IL-17 responses were also decreased. There were sustained decreases in cytokine responses to viral, but not bacterial, stimulants six months after BNT162b2 vaccination. Cytokine responses to irradiated SARS-CoV-2, and spike glycoprotein subunits (S1 and S2) were increased at V2 + 28 for most cytokines and remained higher than pre-vaccination responses 6 months after BNT162b2 vaccination for irradiated SARS-CoV-2 and S1.
“Immune tolerance” is the key phrase here common to all of this. Recent peer reviewed evidence of the boosters is showing the effect of Original Antigenic Sin (OAS) also known as immunological imprinting.
What’s that?
That’s the condition whereby your body’s immune response, generating antibodies, have been reconfigured to only produce antibodies to the Wuhan strain, not able to adapt.
Immunogenicity of BA.5 Bivalent mRNA Vaccine Boosters
Our data indicate that both monovalent and bivalent mRNA boosters markedly increased antibody responses but did not substantially augment T-cell responses. Neutralizing antibody titers against the ancestral strain of SARS-CoV-2 were higher than titers against BA.5 after both monovalent and bivalent boosting. The median BA.5 neutralizing antibody titer was similar after monovalent and bivalent mRNA boosting, with a modest trend favoring the bivalent booster by a factor of 1.3. It is possible that larger studies may show a greater between-group difference, but any such comparative studies between monovalent and bivalent mRNA boosters would need to enroll the two cohorts within the same time frame and after the BA.5 surge, because negative results on nucleocapsid serologic analysis would not exclude all infected participants. These data are consistent with the modest benefits observed with a BA.1-containing bivalent mRNA booster.4 Our findings suggest that immune imprinting by previous antigenic exposure5 may pose a greater challenge than is currently appreciated for inducing robust immunity against SARS-CoV-2 variants.
Source: New England Journal of Medicine
Immunogenicity of the BA.1 and BA.4/BA.5 SARS-CoV-2 Bivalent Boosts: Preliminary Results from the COVAIL Randomized Clinical Trial
Titers against BQ.1.1 and XBB.1 were 8-22 times and 13-35 times lower than against BA.1 and D614G, respectively, with the Wildtype/Omicron BA.1 vaccine. Titers against BQ.1.1 and XBB.1 were 4-12 times and 8-22 times lower than against BA.4/BA.5 and D614G, respectively, with the Wildtype/Omicron BA.4/BA.5 vaccine. However, there was increasing neutralization escape with the late 2022 Omicron subvariants (BQ.1.1 and XBB.1). This escape is similar between the two bivalent vaccines as demonstrated by numerically similar GMTs with overlapping confidence intervals, even though BA.1 and BA.4/BA.5 spike sequences are known to have different mutations in the receptor binding domain.7 Our findings highlight ongoing concern that the breadth of antibody response from current updated vaccines is not optimal for the pace of virus evolution.
Or this preprint awaiting peer review:
Antibody responses to Omicron BA.4/BA.5 bivalent mRNA vaccine booster shot
Boosting with a new bivalent mRNA vaccine targeting both BA.4/BA.5 and an ancestral SARS-CoV-2 strain did not elicit a discernibly superior virus-neutralizing antibody responses compared boosting with an original monovalent vaccine. These findings may be indicative of immunological imprinting, although follow-up studies are needed to determine if the antibody responses will deviate in time, including the impact of a second bivalent booster.
You see, on the road to toleration, the damage to the antibody response has been well documented.
This increased likelihood of infection post booster doses has already been seen in Cleveland Clinic studies where it shows the more shots you take, the more instances of infection you experience.
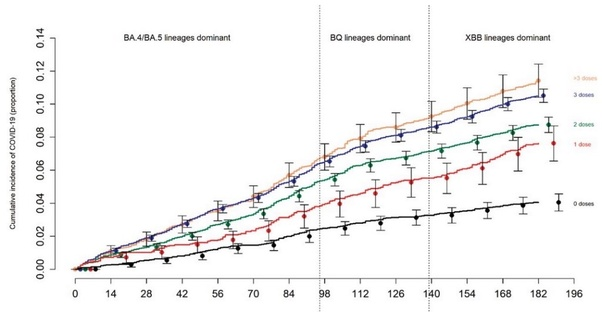
“The association of increased risk of COVID-19 with higher numbers of prior vaccine doses in our study, was unexpected. A simplistic explanation might be that those who received more doses were more likely to be individuals at higher risk of COVID-19. A small proportion of individuals may have fit this description. However, the majority of subjects in this study were generally young individuals and all were eligible to have received at least 3 doses of vaccine by the study start date, and which they had every opportunity to do.”
“Therefore, those who received fewer than 3 doses (>45% of individuals in the study) were not those ineligible to receive the vaccine, but those who chose not to follow the CDC’s recommendations on remaining updated with COVID-19 vaccination, and one could reasonably expect these individuals to have been more likely to have exhibited higher risk-taking behavior.”
“Despite this, their risk of acquiring COVID-19 was lower than those who received a larger number of prior vaccine doses. This is not the only study to find a possible association with more prior vaccine doses and higher risk of COVID-19. A large study found that those who had an Omicron variant infection after previously receiving three doses of vaccine had a higher risk of reinfection than those who had an Omicron variant infection after previously receiving two doses of vaccine [21]. Another study found that receipt of two or three doses of a mRNA vaccine following prior COVID-19 was associated with a higher risk of reinfection than receipt of a single dose [7]”
Another study was therefore carried out to delve into this phenomenon more closely.
Risk of COVID-19 Based on Vaccination Status and Prior Infection
The risk of COVID-19 was lower in the “not up-to-date” state than in the “up-to-date” state, with respect to COVID-19 vaccination (Figure 1). When stratified by tertiles of propensity to get tested for COVID-19, the “not up-to-date” state was not associated with a higher risk of COVID-19 than the “up-to-date” state in any tertile (Figure 2).
DISCUSSION
This study found that not being “up-to-date” on COVID-19 vaccination, using the current CDC definition, was associated with a lower risk of COVID-19 than being “up-to-date”, while the XBB lineages were the dominant circulating strains of SARS-CoV-2.
There are two reasons why not being “up-to-date” on COVID-19 vaccination by the CDC definition was associated with a lower risk of COVID-19. The first is that the bivalent vaccine was somewhat effective against strains that were more similar to the strains on the basis of which the bivalent vaccine was developed, but is not effective against the XBB lineages of the Omicron variant [2]. The second is that the CDC definition does not consider the protective effect of immunity acquired from prior infection. Because the COVID-19 bivalent vaccine provided some protection against the BA.4/BA.5 and BQ lineages [2], those “not-up-to-date” were more likely than those “up-to-date” to have acquired a BA.4/BA.5 or BQ lineage infection when those lineages were the dominant circulating strains. It is now well-known that SARS-CoV-2 infection provides more robust protection than vaccination [4,11,12]. Therefore it is not surprising that not being “up-to-date” according to the CDC definition was associated with a higher risk of prior BA.4/BA.5 or BQ lineage infection, and therefore a lower risk of COVID-19, than being “up-to-date”, while the XBB lineages were dominant.
The strengths of our study include its large sample size, and its conduct in a healthcare system that devoted resources to have an accurate accounting of who had COVID-19, when COVID-19 was diagnosed, who received a COVID-19 vaccine, and when. The study methodology, treating vaccination status as a time-dependent covariate, allowed for determining vaccine effectiveness in real time. Adjusting for the propensity to get tested for COVID-19 should have mitigated against concern that individuals who bothered to remain up-to-date on COVID-19 vaccination may have been more likely to get tested for COVID-19 when they had symptoms.
There are those that say the Cleveland Clinic study “proves the booster works” by showing a 30% RRR relative risk reduction between cohorts. They are, of course, still falling for the RRR efficacy fallacy that trapped them in the beginning through the “95% efficacy at protecting from infection”. The ARR (absolute) risk reduction for the bivalent calculates at -1.5%.
But why stop there! It’s also been observed that there are ‘infection enhancing / non neutralizing antibodies” that increase the infections.
Infection-enhancing antibodies may limit the efficiency of Covid-19 vaccines. We analyzed the evolution of neutralizing and facilitating epitopes in 1,860,489 SARS-CoV-2 genomes stored in the Los Alamos database from June to November 2021. The structural dynamics of these epitopes was determined by molecular modeling of the spike protein on a representative panel of SARS-CoV-2 variants. D614, which belongs to an antibody-dependent-enhancement (ADE) epitope common to SARS-CoV-1 and SARS-CoV-2, has mutated to D614G in 2020, which could explain why ADE has not been detected following mass vaccination. A second epitope located in the N-terminal domain (NTD), specific of SARS-CoV-2, is highly conserved among most variants. In contrast, the neutralizing epitope of the NTD showed extensive variations in SARS-CoV-2 variants. The balance between facilitating and neutralizing antibodies is in favor of neutralization for the Wuhan strain, alpha and beta variants, but not for gamma, delta, lambda, and mu. The recently emerging omicron variant is atypic as its mutational profiles affects both neutralization and ADE epitopes. Overall, our data reveal that the evolution of SARS-CoV-2 has dramatically affected the ADE/neutralization balance. Future vaccines should consider these findings to design new formulations adapted to SARS-CoV-2 variants and lacking ADE epitopes in the spike protein
- SARS-CoV-2 infectivity is enhanced by specific antibodies independent of the Fc receptor
- The open RBD state is induced upon antibody binding to a specific site on the NTD
- Divalent bridging of spikes is required to induce the RBD-up state
- Infectivity-enhancing antibodies are detected in severe COVID-19 patients
So imagine all the spike that have recently been shown to be produced by potentially half of all modRNA for 187 days[10], the antibody response changing the conformational change from closed to open in the jabbed cohort, randomly depleting ACE2 all over the body. And there’s a scary thought. All the while the immune response becomes exhausted through multiple shots, potentially against organs where cells don’t regenerate once destroyed through transfection (heart, or liver if in big enough doses) causing scarring and, in the case of the cardiac system, a dysfunctional rhythm.
Footnotes
- https://www.nejm.org/doi/full/10.1056/NEJMoa2105000
- Age-stratified infection fatality rate of COVID-19 in the non-elderly informed from pre-vaccination national seroprevalence studies
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7947934/pdf/BLT.20.265892.pdf/
- Immune-Mediated Disease Flares or New-Onset Disease in 27 Subjects Following mRNA/DNA SARS-CoV-2 Vaccination - PubMed
- The Emergence of new-onset SLE following SARS-CoV-2 vaccination
- Potential Autoimmunity Resulting from Molecular Mimicry between SARS-CoV-2 Spike and Human Proteins
- Effect of SARS-CoV-2 BNT162b2 mRNA vaccine on thyroid autoimmunity: A twelve-month follow-up study
- Autoimmune hepatitis after COVID-19 vaccination - PubMed
- https://www.researchgate.net/publication/369008110_Emergence_of_Post_COVID-19_Vaccine_Autoimmune_Diseases_A_Single_Center_Study
- https://onlinelibrary.wiley.com/doi/10.1002/prca.202300048
- Deaths by vaccination status, England