Fall of the superorganism: the role of antibiotics in the development of chronic inflammatory pathologies.
*** Abridged version of an essay I wrote during the first semester of my MRes; not a lot of people understand the importance of the bacteria in their body, particularly in their digestive system. Having developed Chrohn's disease after taking tetracycline antibioitcs for ~3 years to treat cystic acne, I thought I would share this.
500 million years of evolution has given rise to the superorganism (Morris et al, 2008; Ley et al, 2008): a host organism whose indigenous metabolic processes have become intrinsically integrated with those of the commensal microbiome living within it (Lederberg et al, 2000; Nicholson et al, 2000). The product of the superorganism is an extensive transgenomic co-metabolism; the presence of which is no more obvious than in the gastrointestinal system. In humans, the extensive gastrointestinal microbiota acts as a “virtual organ”, bestowing metabolic function beyond the capability of our own limited metabolic physiology; allowing digestion of complex plant polysaccharides and synthesis of essential vitamins. Some organisms that colonise our body are ingrained in our development as a species, so much so, that those such as Helicobacter pylori strain diversity can be used to track the migration of early humans out of Africa (Falush et al, 2003).
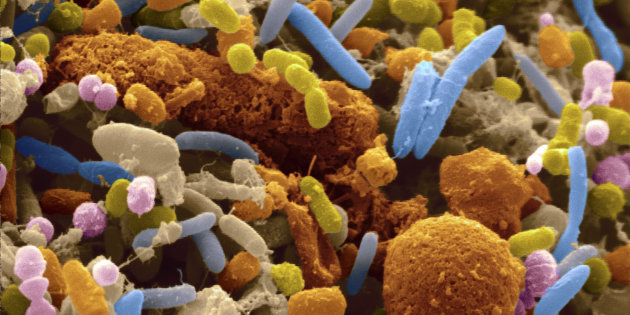
The role of the gut microbiome in maintaining the health of an individual is becoming increasingly evident, with increasing reports of dysbiosis of microbiome associated with obesity (Cani et al, 2008), type-2 diabetes (Qin et al, 2012), autism spectrum disorders (de Theije et al, 2014), but most obviously, in the development of inflammatory bowel disease (IBD): Crohn’s disease and ulcerative colitis (Manichanh et al, 2006; 2012; 2014; Dicksved et al, 2008; Asquith et al, 2010). IBD sits at the core of a number of immune mediated diseases, with sufferers significantly more likely to develop arthritis, psoriasis, and bowel cancer. Worryingly, the incidence of IBD has been increasing steadily since the end of WWII, the cause of which is unclear, however is associated with a dramatic change in lifestyle, particularly in the western world. Of these factors, the most heavily implicated is the increasing use of antibiotics in young children.
No environmental factor displays a more devastating effect on gut microbial diversity than the long-term or regular use of antibiotics, which diminish overall population sizes of necessary commensal bacteria, and subsequently allows an increase in proliferation of fungi and pathogenic bacteria. Antibiotics may also contribute to a selective pressure increasing prevalence of antibiotic resistant wall-deficient L-form bacteria; the relationship between IBD and L-form bacteria has been documented for decades (Parent et al, 1976; Belshein et al, 1983; Chiodini et al, 1986), however it was never clear whether these bacteria contributed to the development of the disease, or were simply a consequence of it. As these bacteria lack a cell wall, they are intrinsically immune to conventional penicillin based antibiotics, and with increasing evidence of a relationship between antibiotics and IBD (Card et al, 2004; Margolis et al, 2010; Kronman et al, 2012), one may speculate that those two factors (antibiotics and L-form bacteria) go hand in hand in acting as causative agents for development of IBD.
Unfortunately, to date, most research into association of dysbiosis of gut microbiome with IBD has been descriptive: characterising associations using cohort data or small scale medical trials, thus leaving researchers unable to conclude any distinct cause and effect relationship, or to elucidate the molecular mechanisms by which dysbiosis of the gut microbiome cause immune aberrations. The reason for a lack of understanding in this area may simply be due to the difficulty in conducting a study using human subjects, particularly due to the fact that the underlying mechanisms of chronic inflammatory pathologies are still vague. What is clear, however, is that it would be wise for individuals to avoid the use of antibiotics, particularly for prolonged periods.
References
Asquith, M. and Powrie, F. (2010) ‘An innately dangerous balancing act: intestinal homeostasis, inflammation, and colitis-associated cancer’, The Journal of Experimental Medicine, 207(8), pp. 1573–1577.
Belsheim, M. R. et al. (1983) ‘Bacterial L-form isolation from inflammatory bowel disease patients’, Gastroenterology, 85(2), pp. 364–369.
Bresciani, A. et al. (2016) ‘The Mouse Intestinal Bacterial Collection (miBC) provides host-specific insight into cultured diversity and functional potential of the gut microbiota’, Nature Microbiology, 1(10), p. 16131.
Cani, P. D. et al. (2008) ‘Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice’, Diabetes, 57(6), pp. 1470–1481.
Card, T. et al. (2004) ‘Antibiotic use and the development of Crohn’s disease’, Gut, 53(2), pp. 246–250.
Chiodini, R. J. et al. (1986) ‘Spheroplastic phase of mycobacteria isolated from patients with Crohn’s disease.’, Journal of Clinical Microbiology, 24(3), pp. 357–363.
Dicksved, J. et al. (2008) ‘Molecular analysis of the gut microbiota of identical twins with Crohn’s disease’, The ISME journal, 2(7), pp. 716–727.
Domínguez-Cuevas, P. et al. (2012) ‘The rod to L-form transition of Bacillus subtilis is limited by a requirement for the protoplast to escape from the cell wall sacculus’, Molecular Microbiology, 83(1), pp. 52–66.
D’Incà, R. et al. (2008) ‘Can calprotectin predict relapse risk in inflammatory bowel disease?’, The American Journal of Gastroenterology, 103(8), pp. 2007–2014.
Falush, D. et al. (2003) ‘Traces of human migrations in Helicobacter pylori populations’, Science (New York, N.Y.), 299(5612), pp. 1582–1585.
Gevers, D. et al. (2014) ‘The treatment-naïve microbiome in new-onset Crohn’s disease’, Cell host & microbe, 15(3), pp. 382–392.
Harrelson, W. G. and Mason, R. P. (1982) ‘Microsomal reduction of gentian violet. Evidence for cytochrome P-450-catalyzed free radical formation.’, Molecular Pharmacology, 22(2), pp. 239–242.
Henriksen, M. et al. (2008) ‘C-reactive protein: a predictive factor and marker of inflammation in inflammatory bowel disease. Results from a prospective population-based study’, Gut, 57(11), pp. 1518–1523.
Kim, B.-S., Kim, J. N. and Cerniglia, C. E. (2011) In Vitro Culture Conditions for Maintaining a Complex Population of Human Gastrointestinal Tract Microbiota.
Kronman, M. P. et al. (2012) ‘Antibiotic Exposure and IBD Development Among Children: A Population-Based Cohort Study’, Pediatrics, pp. peds.2011–3886.
Lederberg, J. (2000) ‘Infectious history’, Science (New York, N.Y.), 288(5464), pp. 287–293.
Ley, R. E. et al. (2008) ‘Worlds within worlds: evolution of the vertebrate gut microbiota’, Nature Reviews. Microbiology, 6(10), pp. 776–788.
Manichanh, C. et al. (2006) ‘Reduced diversity of faecal microbiota in Crohn’s disease revealed by a metagenomic approach’, Gut, 55(2), pp. 205–211.
Manichanh, C. et al. (2012) ‘The gut microbiota in IBD’, Nature Reviews. Gastroenterology & Hepatology, 9(10), pp. 599–608.
Manichanh, C. et al. (2014) ‘Anal gas evacuation and colonic microbiota in patients with flatulence: effect of diet’, Gut, 63(3), pp. 401–408.
Margolis, D. J. et al. (2010) ‘Potential Association Between the Oral Tetracycline Class of Antimicrobials Used to Treat Acne and Inflammatory Bowel Disease’, The American Journal of Gastroenterology, 105(12), p. 2610.
Mercier, R., Kawai, Y. and Errington, J. (2013) ‘Excess Membrane Synthesis Drives a Primitive Mode of Cell Proliferation’, Cell, 152(5), pp. 997–1007.
Morris, S.C., and Peel, J.S. (2008) The earliest annelids: Lower Cambrian polychaetes from the Sirius passet lagerstatte, peary land, north Greenland. Acta. Palaeont. Polon. 53, 137-148.
Nicholson, J. K., Holmes, E. and Wilson, I. D. (2005) ‘Gut microorganisms, mammalian metabolism and personalized health care’, Nature Reviews. Microbiology, 3(5), pp. 431–438.
Parent, K. and Mitchell, P. D. (1976) ‘Bacterial Variants: Etiologic Agent in Crohn’s Disease?’, Gastroenterology, 71(2), pp. 365–368.
Qin, J. et al. (2012) ‘A metagenome-wide association study of gut microbiota in type 2 diabetes’, Nature, 490(7418), pp. 55–60.
Stidolph, N.E., Alston, J.M. (1960) The use of soframycin (farmycetin sulphate) for intestinal sterilization. Gut. 1, pp. 323-325.
de Theije, C. G. M. et al. (2014) ‘Altered gut microbiota and activity in a murine model of autism spectrum disorders’, Brain, Behavior, and Immunity, 37, pp. 197–206.