Superbug: The End of Antibiotics? Are We All Going to Die?
What on Earth is a superbug?
Imagine having an incurable bacterial infection that doctors can't stop from spreading. How long have you got to live? You are asking yourself, how this can be possible in the 21st century. The era of the superbug has dawned upon us. According to the Centers for Disease Control and Prevention (CDC), about 2 million people get sick from a superbug every year, out of which 23,000 die.
How super is a superbug?
The term ‘superbug’ is a sensational one that has been coined by the media because it resonates by creating fear. We all know how the media loves a little bit of drama right? Brian K. Coombes, PhD, of McMaster University in Ontario explains:
And yes, on the 27th of May the case of a 49 year old woman with a superbug that beat even the last-resort antibiotic was all over the news:Doctors often use phrases like "multidrug-resistant bacteria." That's because a superbug isn't necessarily resistant to all antibiotics. It refers to bacteria that can't be treated using two or more.
However as the article on CNN’s website shows, it all ended well:
So no big deal right?
Wrong! Let’s not even think of belittling the situation. The threat is real, and 23,000 deaths a year is no joke. Besides, antibiotics are the backbone of modern medicine. Here is more from Brian K. Coombes:
Cancer chemotherapy, organ transplants, surgeries, and childbirth all rely on antibiotics to prevent infections. If you can't treat those, then we lose the medical advances we have made in the last 50 years.
How do I protect myself from a superbug?
1. Avoid antibiotic misuse
Do not misuse antibiotics by taking them when you don't need them or by not finishing all of your medicine. According to the CDC, this is the "single leading factor" contributing to this problem. Also know that the more antibiotics you’ve taken, the higher your risk of catching a superbug.2. Stay alert in hospitals
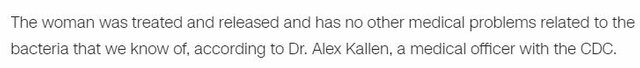
The hospital is also a high-risk place to be. The more visits you to the hospital setting, the more you risk catching a superbug. In the hospital environment, you may catch a superbug through what experts call ‘healthcare-associated infections’ (HAIs). According to the CDC,” Many of the most urgent and serious antibiotic-resistant bacteria threaten patients while they are being treated in healthcare facilities for other conditions, and may lead to sepsis or death.” So make sure the doctors and nurses are following the right protocol to avoid infections.Please see the CDC infographic below:
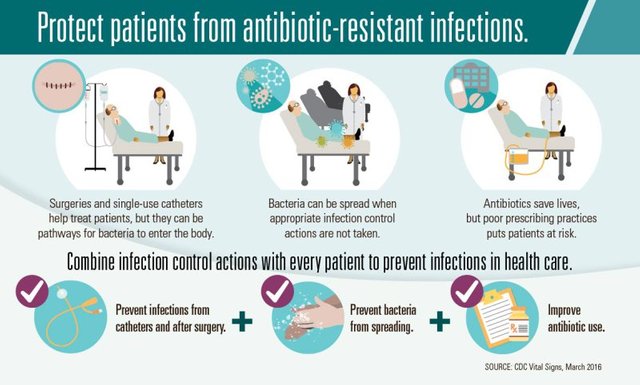
3. Avoid antibiotic-tainted meat
The use of antibiotics in farm animals leads to an increased risk of antibiotic resistant infections in humans. Get your meat from your local farmers, it may be more expensive but it tastes better and is much safer.
What can science do to fight antibiotic resistance?
Anya Vanecek put this question out on Quora and we found the best answer for you. Mary Bushman who does research on resistance in malaria had the best answer. I have put it down word for word:
There are multiple ways we can manage antibiotic resistance. The following is a mix of current, well-accepted methods, as well as some ideas that are still being explored/tested.
1. Preserve the effectiveness of the drugs that still work
(a) Limit use of antibiotics (agricultural use and inappropriate prescribing, as well as over-the-counter availability in many countries) and encourage correct use (finishing the course of treatment).
(b) Prevent resistant bugs from infecting others (infection control in clinical settings, plus regular public health interventions to reduce transmission).
(c) Combination therapy - treating with multiple drugs simultaneously. Using two or more drugs makes it harder for resistance to emerge, since the bug would have to develop resistance to both drugs.
(d) Vary the selection pressure. The more consistently a drug is used, the more advantage there is in being resistant. Using a variety of drugs (by giving different drugs to different people or switching the "drug of choice" every few years) may help prevent or reduce resistance.
2. Develop new drugs
(a) Find drugs with mechanisms of action (ways of killing) that don't overlap with current drugs. When drugs share a mechanism, resistance to one will often mean resistance to the other. Finding drugs that work in different ways helps avoid this, and also works better for combination therapy.
(b) Search for drugs that are hard to develop resistance to. As we learn more about how different drugs kill, and how resistance works, drug development can be smarter and more targeted (as opposed to random screening of thousands of compounds for antibiotic activity).
(c) Unfortunately, developing new drugs is expensive, and pharmaceutical companies weigh the cost of development against a new drug's money-making potential. We badly need new drugs for malaria and tuberculosis, but since these are mainly diseases of "poor people" who can't afford expensive new drugs, pharm companies consider it a bad investment.
3. Try to reverse existing resistance
(a) In some cases, when a drug stops being used because of resistance, the resistance will actually start to go back down. This is because of a "cost" of resistance, meaning when the drug is not there, the resistant types don't do very well. An example is that chloroquine-resistant malaria is present in many places, but in a number of places where chloroquine is no longer used, the resistance has decreased. If we can control drug use enough to make this happen, we may be able to "save" some drugs that are losing their effectiveness.
(b) In some cases, there can be a "trade-off" with resistance to different drugs. You can be resistant to drug A, or to drug B, but not both. If resistance to drug A is very common, and you start treating everyone with drug B, the bug might evolve resistance to B, but would have to lose the resistance to A. So, you might be able to start using A again in the future. This won't happen in every case, or even very often, but when it does happen it can be a neat solution.
See the original answers to”How do we solve antibiotic resistance?”
Conclusion
So we can conclude that antibiotic resistance is not the end of antibiotics. The superbug that just came to the U.S. is still treatable as I explained. We have been creating more and more resistant strains by misusing antibiotics, be it through direct consumption or through farm animals. Perhaps someday all bacteria will be resistant to all types of current antibiotics, but that just means we will have to discover a new type of cure.
Source: