Alterations in Gastrointestinal Function- GASTROINTESTINAL BLEEDING !

Gastrointestinal bleeding is a very important health problem both in terms of clinical diagnostically and therapeutically, most experts considered it a surgical emergency.
Bleeding gastrointestinal bleeding are considered externalized, as the blood drains into a hollow organ belonging to the digestive tract, be it the esophagus, stomach, or intestine and is then externalized by hematemesis, melena, rectal bleeding.
Major bleeding and acute hemodynamic events are accompanied by, the most serious being hypovolemic shock.
Gastrointestinal haemorrhages are classified according to several criteria, as follows: depending headquarters and duodenal-jejunal angle ratio (Treitz ligament) are two major types:
- Upper gastrointestinal bleeding (upper angle) including: esophagus, stomach, duodenum
- Lower gastrointestinal bleeding (low angle) comprising small intestine and large intestine.
This classification shows how externalizing clinical importance because it is often suggestive of bleeding actual location.
First bleeding coming from the tube may be signs of digestive cancers (especially stomach) or may occur in the context of caustic injuries. The most common causes of upper gastrointestinal bleeding are peptic ulcer, gastritis, esophageal varices, Mallory- Weiss syndrome.
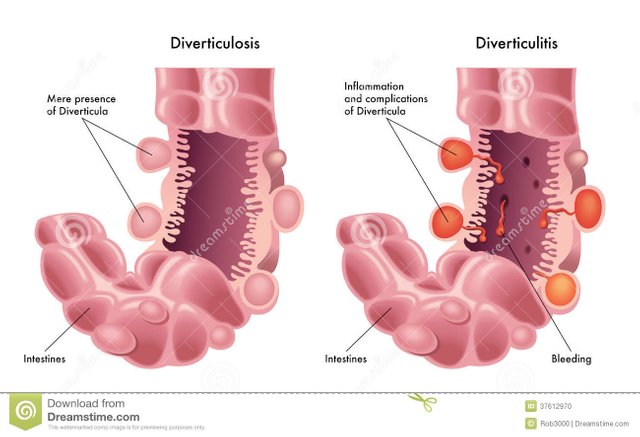
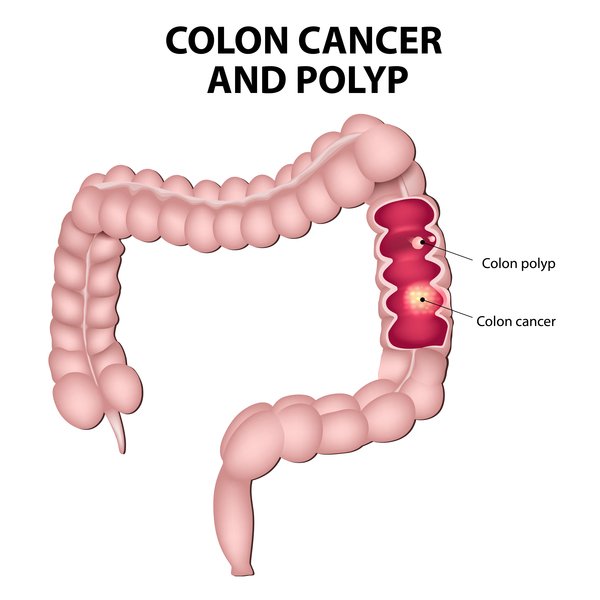
Lower digestive bleeding are those that reflect the suffering of the gastrointestinal tract distal angle, including small intestine, large intestine, rectum and anus. Occur more frequently in diverticular disease (diverticulosis / diverticulitis), polyps, hemorrhoids and anal fissures. Also, the blood may be present in the stool and the processes neoplastic, inflammatory (Crohn's disease) but can occur in infectious diarrhea.
Causes
Upper gastrointestinal bleeding
Theoretically, causes upper gastrointestinal bleeding in general differ from those of lower bleeding so:
Peptic ulcer disease - account for about 40% of cases of bleeding. The disease is characterized by erosive lesions of the mucous membrane and its underlying structures, depending on the severity. Predilection are the stomach and duodenum. As the project progresses deeper structures are affected mucosa, submucosa, and blood vessels, causing bleeding their erosion. The main factor is aggressively vessels increased gastric acidity (gastric juice exerts a direct effect on vascular walls, with their subsequent erosion). There are a number of factors that favor ulcers consumption of NSAIDs (mainly aspirin in large quantities), alcohol, tobacco. The drugs work by lowering defense capacity of the gastric epithelium (interfering with mucus and bicarbonate secretion that are protective against clorhidropeptica acidity). Another factor is frequently incriminated Helicobacter pylori, a bacterium that is found in the mucus layer on the surface of gastric epithelium. This decreases considerably the mucosal defense, making a favorable ground installation ulcers.
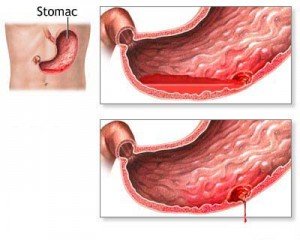
Erosion gastritis: gastritis is inflammation of the stomach wall and engineering may be complicated by bleeding. It is caused by insufficient function of defense mucus layer, hydrochloric acid can easily damage such vessels. Factors favoring the occurrence of gastritis are: NSAIDs, corticosteroids, alcohol, burns, injuries.
Esophageal varices: are No. 3 in frequency of digestive diseases that cause upper gastrointestinal hemorrhage, but the intensity is major bleeding. Varicose veins are caused by changes in pressure in the portal circulation and is in the form of the path vascular dilatation. Esophageal varices occur in liver disease (90% are caused by cirrhosis of the liver, this being mainly alcoholic etiology). Experts believe that there are two mechanisms breaking veins: through erosion or as a result of sudden pressure changes. Bleeding from varices can be severe, it occurs without premonitory signs and its treatment is very complex.
Mallory-Weiss syndrome: tear the lining of the lower esophagus, the eso- gastric or stomach lining occurs after intense efforts of coughing, vomiting, seizures, defecation or during labor. Such injuries can be detected in patients with a recent history of excessive drinking and alcohol abuse. Mucosal bleeding laceration represents 3% of upper gastrointestinal bleeding.
Lower gastrointestinal bleeding
Common causes of lower gastrointestinal bleeding:
Diverticulosis: is one of the most common causes of lower bleeding. Pouches that characterize this disease is actually small bags or exvaginari a few millimeters to several centimeters, which is formed by lining herniation outside the lumen of the colon, especially weaknesses, namely in places where vessels penetrate the wall. Their number is variable and is much higher in people who have chronic constipation.
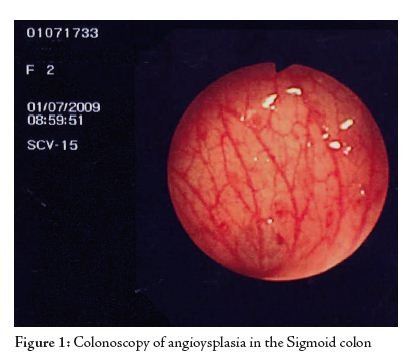
Angiodysplazia: angyodisplazia is the second leading cause of lower gastrointestinal bleeding (in terms of frequency). It is a vascular malformation of the intestine nature underlying the occurrence of bleeding and anemia. Angiodisplazice lesions are usually multiple and have favorite location at the check and ascending colon (but not exclusively here). It seems that such defects are more common in elderly patients and in those with chronic kidney disease.
Polyposis: intestinal polyps are benign tumors of the gastrointestinal tract that occur with higher frequency in people over 40 years. Bleeding from polyps can be acute signs and symptoms frustrating manifest and intense, or it can be chronic, with a long evolution and occult character. Polyps shows some risk of malignancy.
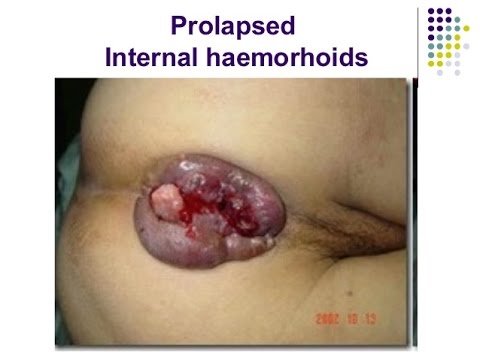
Hemorrhoids and anal fissures: Hemorrhoids are actually swollen varicose dilations of the veins that drain the rectum and is a fairly common disorder, experts estimating that about 50% of the entire population of the planet will develop the disease during their lives. Anal fissures or lacerations of the wall may be caused by the presence of blood in the stool or bleeding in his absence. Lacerations occur during intense efforts of defecation (chronically constipated patients).
Symptoms
Symptoms of gastrointestinal bleeding and semiotics is varied and generally depends on the amount of blood lost, the time is lost and digestive segments concerned. Thus, acute, severe bleeding may have serious repercussions and systemically important echoes in hypovolemic balance the body's minor compared to the chronic and which is manifested by anemia well tolerated by the individual. Locating front ligament Treitz is important in clinic because bleeding Superior externalized most frequently by hematemesis (vomiting blood digest, with the appearance of coffee grounds) and faecal occult blood (removing the stool black and shiny as oil) and the lower form the rectal.
Symptoms associated with blood loss in the digestive track include: fatigue, chronic anemia, fatigue, dyspnea (difficulty breathing) or dark stools positive for fecal occult bleeding if the long term.
If blood loss is massive and acute, the patient can go into hypovolemic shock (a life-threatening situation) and should be rebalanced immediately otherwise the risk of death is very high.
Specialist advice
The doctor should consulted immediately if the patient noticed the presence of blood franc in the stool or any change in color (brown, black shiny) and consistency (seats Melena are softer than normal because blood in the gastrointestinal tract is a powerful stimulator of intestinal peristalsis).
Patients also are advised to consult your doctor when blood vomit, feel dizzy and powerless, you quickly tire performing usual activities.
Digestive bleeding are considered surgical emergencies as they may have vital risk, which is why patients are advised to give them the necessary attention and present timely emergency department specialist for investigation and treatment.
Investigations
The doctor will perform a patient's complete history and physical examination in order to decide what general investigations are needed to finalize the diagnosis. Some mandatory physical examination is conducting a digital rectal exam (to detect bleeding in the lower, especially anal canal and rectum).
Necessary and important steps in investigating their digestive bleeding is conducting esofagogastroduodenoscopiei or colonoscopy (depending on the signs) and laboratory tests that aim to determine the body's response to blood loss and its direct consequences on its functions.
- Endoscopy is the process in which the doctor inserted through the mouth to the stomach a flexible tube fitted at one end with a video camera to provide images about the integrity of the upper segments of the digestive tract. It is considered to be a minimally invasive technique because it does not necessitate special incisions and does not require a long recovery (unless that was done under general anesthesia). Upper endoscopy can detect digestive bleeding easily place and even has therapeutic use and can be used to stop bleeding during office accessible to small intervention with hemostatic role.
- Colonoscopy is all but a maneuver endoscopic colonoscopy, flexible plastic tube equipped with a video camera, is inserted through the anus and rectum and examines the colon, can reach even up to the ileocecal valve.
- Laboratory tests are centered on CBC, with emphasis on hematocrit, hemoglobin, red blood cell counts (anemia eventual objective to what may occur in acute or long). If not detected the source of bleeding is analysis occult seat.
Specialized treatment
Specialized treatment for bleeding gastrointestinal is complex and varies depending on the actual location of bleeding and bleeding intensity. In severe cases may occur hypovolemic shock patients requiring resuscitation and volume replacement rebalancing. In such situations is given intravenous fluids and blood transfusions.
Other therapeutic measures include:
- Administration of proton pump inhibitors to reduce stomach acid and stop a possible chemical attack on the blood vessels in case of upper gastrointestinal hemorrhage
- Correction of coagulopathy by administering vitamin K or fresh plasma
- Reducing portal hypertension, in case of bleeding oesophageal varices by administering vasopressin analogue octreotide and rarer.
Severe cases with rapid deterioration of general condition of the patient and are operated life-threatening emergency.
Special Recommendations
Experts recommend patients to have a proper diet and avoid excessive alcohol consumption, food that favors constipation (predominantly regime sausage) and follow proper physician advice, especially regarding drug administration.
Patients must present further medical checks regularly to monitor progress and cure them and to be able to detect early any complications of gastrointestinal bleeding.
Preventions
There are certain hygienic dietary measures can prevent gastrointestinal bleeding by avoiding the installation of some of the causes:
- Avoid spicy foods, smoking, excessive alcohol consumption and all the factors that lead to increased gastric secretions
- Consumption of foods rich in fiber stimulates peristalsis, favors the formation and elimination of soft stool, preventing constipation which can subsequently lead to diverticular disease and hemorrhoids.
Source:
1. Baum S, Nusbaum M, Clearfield HR et al – Angiography in the diagnostic of gastrointestinal bleeding.
2. Becouarn Y, Lamouliatte H, Quinton A – Lésion aiguës de l’oesophage d’origine medicamenteuse
3. Berman St – Hematemesis.
4. Roy CC, Silverman A – Gastrointestinal bleeding. In: Kempe CH, Silver HK, O’Brien.
5. Perelman R, Jos J – Hémorragies digestives.
Also Look on :
https://steemit.com/medicine/@nelu.ceban/alterations-in-gastrointestinal-function-dysphagia