The Genetic Reprogram of Stem Cells
Disclaimer
This scientific-themed paper is abstract by nature, and should not be considered empirical evidence as proof the reprogram process of stem cell DNA is credible and/or possible. The purpose of the paper is meant to express an idea worth sharing with the general public, regardless of individual intelligence to readily understand. I don’t claim ownership of the idea should anyone wish to undergo an attempt to experiment whether or not the reprogram process of stem cell DNA is possible. I am not responsible for any misguidance, miscommunication, injury or death of life whether human or not, loss of monetary resources and/or property, and mistakes carried out by all parties who began research from an idea derived from this paper. I am only responsible for the public release of this paper. I am the original author of this paper, meaning no other parties can claim original ownership as the mastermind.
Joel Hovell ~ October 6th, 2018
Introduction
In August of 2017, there were over 114,000 people registered on the national transplant waiting list. Eighty-three percent of them continue to wait for someone with a match in order to receive a kidney transplant, which is a significant number compared to the need for liver transplants at 12.1%.1 The need for organ donors will continue to outweigh those in need of an organ transplant since numbers were kept starting in 1991 as shown in Figure 1. In addition to these statistics, the elderly population of the United States, those aged 65 years and older, stood at 44.5 million as of 2013, with data showing that this number will continue to increase over the next four decades.3 Similar to those in need of an organ transplant, organs in those part of the elderly population have reduced efficiency, or a complete lack of benefit due to organ failure. Is the observance of loved ones die before us through natural degradation of our
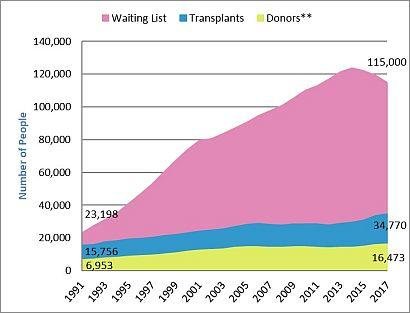
Figure 1. Organ Shortage 1991-2017.2
**Data includes deceased and living donors.
natural wireframe something we should expect anymore? Scientists around the world have considered to engage in research meant to list the aging process, not to mention those through genetic defect who need an organ transplant not due to aging, as an illness with a wide variety of triggers worth treating. However, to treat the aging population by a reversal in genetic damage and organ transplant, remains unavailable.
With a recent advancement in the transformation of skin cells into induced pluripotent stem cells conducted by Professor Timo Otonkoski, University of Helsinki, Professor Juha Kere, Karolinska Institutet and King’s College London, and their team of researchers, a gap has been bridged in the ideal to treat an aging population and those in need of an organ transplant.4 A potential goal going forward would be to discover a method of effective means to alter the DNA of induced pluripotent stem cells to match a patient’s DNA. This would allow for scientists to create healthy organs and cells from healthy donor stem cells derived from skin cells. However, there is a possibility to also use cheek cells as described in a lecture by Shinya Yamanaka featured in the YouTube video Stem cells - the future: an introduction to iPS cells.5
Collection Phase
At the time of writing, the transformation of skin cells into induced pluripotent stem cells is one of the most recent advances in order to create stem cells from other types of cells in the human body. This is achieved by the collection of skin cells from an individual, followed by the activation of certain genes. These genes, specifically proteins, were first discovered by Shinya Yamanaka in 2007, a stem cell researcher who is currently affiliated with Kyoto University, and the Gladstone Institutes.6,7 This will be explained in detail in the next section; Reprogram: Phase 1.
Another method to create stem cells from other types of specialized cells is the choice to use cheek cells. This was described in a lecture performed by Shinya Yamanaka featured in a YouTube published in 2012.5 In the lecture, a video was shown of a collection of heart cells beating that had been originally created from a sample of a 36-year-old woman’s cheek cells. With the activation of certain genes the cheek cells were transformed into induced pluripotent stem cells followed by a transformation into heart cells. Again, the transformation of cells will be explained in detail in the next section; Reprogram: Phase 1.
The collection of skin cells is typically done through a skin biopsy, and is done by a doctor. The conventional reasons for a skin biopsy to be carried out are to understand whether or not a patient has skin cancer, an infection, or a disorder. There are four techniques to complete a skin biopsy: a shave biopsy, punch biopsy, excisional biopsy, and incisional biopsy.8 A hypothesis must be formed, as the collection technique to collect skin cells for transformation into stem cells is unknown to the general public, it is believed that a shave biopsy would be considered the optimum technique in this case. To support the hypothesis, the integumentary system, skin, is comprised of three main layers. These sections are the epidermis, dermis, and the hypodermis layers.9 Cells from the hypodermis layer shouldn’t be collected because this layer contains adipocytes; or fat cells.9 Although fat cells have been reprogrammed into stem cells, fat cells, obviously, are not skin cells.

Figure 2. Shave Biopsy Tool.11
A shave biopsy is carried out usually by a doctor, though for the purpose of collecting skin cells for transformation into induced pluripotent stem cells, a nurse could be trained. The biopsy is a safe, simple procedure that can be done at a doctor’s office, or potentially at a collection center similar to a plasma donation center. A double-edged blade held with two fingers should be enough to collect the skin cells from the epidermis layer for use to make into stem cells. The advantage of the collection of skin cells from the epidermis layer is that donors would have the convenience to set up appointments that may be no longer than twenty minutes; which includes a brief screening period when the donor first arrives at the center. A second employee would be responsible for the screening process, and would hand the donor off to an awaiting nurse to collect the skin cells through a shave biopsy in a booth with a privacy curtain or enclosed room.
A cheek swab can be done by any medical employee, meaning the person doesn’t necessarily have to be a doctor or a nurse.10 Preferably, this sample can be collected by a phlebotomist, as the swab is fairly easy to complete. The cheek swab is carried out by using a cotton-tipped wooden swab, and placed inside of a plastic container for storage.
Following the collection of cells from a donor, the cells would be stored in the center laboratory. On a daily basis, cell donations will be shipped to the nearest regional laboratory where quality tests are conducted. Once samples are tested and considered safe for medical use, the donated cells will be transferred to research and development.
Reprogram: Phase 1
To undergo the transformation from skin or cheek cells, known as specialized cells, to induced pluripotent stem cells, four proteins must be exposed to the specialized cells. First identified by Shinya Yamanaka in 2007, the proteins Oct4, Sox2, cMyc, and Klf4, were used as they were found to be expressed in large numbers in embryonic stem cells. However, later studies have found that the proteins cMyc and Oct4 can cause cancer when they are over expressed. This problem was overcome by the replacement of the protein Oct4 with the protein NKX3-1.6 Although continued research will be necessary to make the transformation safe, quick, and effective, this change in proteins used for the transformation is a huge step forward in stem cell research.
With the activation of particular genes within the specialized cells, like the skin and cheek cells, using a gene editing tool, such as CRISPR/CAS9, the process to turn these type of cells back into pluripotent stem cells is made easier. This technique was carried out by Professor Timo Otonkoski of the University of Helsinki, Professor Juha Kere of the Karolinska Institutet and King’s College London, along with their team of researchers.6 According to the evidence found online, it has been made uncertain whether or not the same gene were activated to create. However, if the proteins Sox2, cMyc, Klf4, and NKX3-1, through several experiments, have proven to be effective in the creation of induced pluripotent stem cells, there is no evidence proving these were the proteins, or genes, activated. Regardless of what genes inevitably will be activated in order to create stem cells, the reprogram of specialized cells, such as cheek and skin cells, is necessary for the second phase of the reprogram process.
Once samples of donors’ skin or cheek cells have arrived at a research and development facility to begin the process of transformation into induced pluripotent stem cells, the individual samples will need to be isolated from one another. This is done in order to to keep the individual DNA of each sample from being compromised. In individual-sized processes, the specialized cells will undergo the transformation into induced pluripotent stem cells. Research scientists, along with their research assistants, will keep watch twenty four hours a day, seven days a week, to maintain integrity of each of the developing stem cells samples. Although the length of time needed to make the transformation happen is unknown to the general public, it didn’t happen overnight.
Reprogram: Phase 2
To match a patient’s DNA with those of donated specialized cells transformed into induced pluripotent stem cells, the new stem cells must be genetically edited. A gene editing tool, known as CRISPR/CAS9, has been popular with most researchers who specialize in the field of genetics. However, there is a major problem with this genetic tool. CAS9 cuts strands of a DNA molecule that leave blunted ends, which are not easy to work with. CRISPR/CPF1 on the other hand, a newly developed gene editing tool, is able to leave ‘sticky ends,’ which according to synthetic biologist Feng Zhang, is more controllable to insert DNA.13 Although small changes to human DNA have been made primarily by CRISPR/CAS9, CPF1 may hold the key to several hundred changes at once. If CPF1 is unable to change human DNA at this scale, much less several thousand or million changes, continued research will discover a gene editing tool able to overcome this challenge.
Once a sample of induced pluripotent stem cells have adopted a patient’s DNA through gene editing, the process to increase the number of cells begins. Unfortunately, this is another hurdle researchers must overcome before medical advances can occur. There are no scientific papers describing the ability to rapidly increase the number of stem cells with the exception of one. Chengcheng Zhang, a researcher working at the Whitehead Institute, discovered a way to multiply hematopoietic stem cells by 30 times. He accomplished this by adding three growth factor proteins to a sample of hematopoietic stem cells, IGF-2, Angiopoietin-like 2, and Angiopoietin-like 3.14 Although is a noteworthy advancement in stem cell research to increase the number of induced pluripotent stem cells using a similar approach remains incomplete.
The ability to edit large portions of human DNA remains out of reach, and will remain this way for several years. To bring things into perspective, three statistics about human beings must be introduced to show how difficult the task to transform DNA of the donor into that of the patient’s is. There are 3.2 billion base pairs, or genetic letters, that form the human genome. Although according to a 2012 publication by the National Institute of General Medical Sciences, the DNA of most individuals are 99.6 percent identical. This leaves approximately 0.4 percent, or about 12 million base pairs, that are not identical.15 No gene editing tool, as of October of 2018, has been used to edit several million base pairs part of the human genome. This is enough to show this type of stem cell research has a long waiting period before success is achieved.
A New Future
With continued research and development in the field of genetics, the ability to treat patients of old age and/or in need of an organ transplant will be in reach in the coming decades. The ability to transform the aging population into healthy, young individuals would allow them to escape the perils of illnesses such as Parkinson’s Disease, Dementia, heart disease, arthritis, and the like. The ability to heal those in need of an organ transplant would be one of the best gifts one can receive. However, many will say, the human population will increase in number, and there is little space for everyone now. Would not overpopulation become more of a problem should the old become young again while new members of humanity are born too? Although this is a concern, should we pursue the choice to make people young and healthy again, would we want our elders to suffer in agony? Most would describe how they would wish the opposite for their loved ones.
I want everyone to remember, this is a paper that is abstract by nature, and should not be considered empirical evidence as proof the reprogram process of stem cell DNA is credible and/or possible. There is more research required to advance this type of medical science, and it will require hundreds, if not thousands, of people to make the research happen. This paper is about publishing the idea we may possess the power to use our ingenuity to solve medical problems such as creating new organs from donated cells later reprogramed back into stem cells. I want to thank everyone for their time in reading this paper, and have yourselves a wonderful day.
Sources
1.) “Organ Donation Statistics.” Organ Donor, US Department of Health & Human Services, www.organdonor.gov/statistics-stories/statistics.html.
2.) “Organ Donation and Transplantation Statistics: Graph Data.” Organ Donor, US Department of Health & Human Services , www.organdonor.gov/statistics-stories/statistics/data.html.
3.) Burton, James. “The US States With the Oldest Populations.” WorldAtlas, WorldAtlas, 6 Jan. 2016, www.worldatlas.com/articles/the-us-states-with-the-oldest-population.html.
4.) University of Helsinki. "New method for turning skin cells into pluripotent stem cells." ScienceDaily. ScienceDaily, 6 July 2018. www.sciencedaily.com/releases/2018/07/180706091723.html.
5.) Blackburn, Professor Clare, et al. Stem Cells - the Future: an Introduction to IPS Cells. Performance by Professor Shinya Yamanaka, et al., Stem Cells - the Future: an Introduction to IPS Cells, EuroStemCell, 24 Oct. 2012, www.youtube.com/watch?v=Q9-4SMGiKnE.
6.) Conger, Krista. “Researchers Identify Protein Essential for Making Stem Cells.” Phys.org - News and Articles on Science and Technology, Nature Cell Biology, Stanford University Medical Center, 17 July 2018, phys.org/news/2018-07-protein-essential-stem-cells.html.
7.) Shinya Yamanaka – Nobel Lecture. NobelPrize.org. Nobel Media AB 2018. Wed. 10 Oct 2018. https://www.nobelprize.org/prizes/medicine/2012/yamanaka/lecture/.
8.) Staff, Mayo Clinic. “Skin Biopsy.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 17 May 2018, www.mayoclinic.org/tests-procedures/skin-biopsy/about/pac-20384634.
9.) Bailey, Regina. “Integumentary System and Skin Layers.” ThoughtCo, Dotdash Publishing, www.thoughtco.com/integumentary-system-373580.
10.) Farrer, Angela, and S. Pike. “What Is a Cheek Swab?” WiseGEEK, Conjecture Corporation, 17 Sept. 2018, www.wisegeek.com/what-is-a-cheek-swab.htm.
11.) Price, Karen. “Shave Biopsy Tool.” Karen price blog, Women in General Practice Conference 2014, Aug. 2014, karenpriceblog.files.wordpress.com/2014/08/shave-biopsy.jpg?w=231&h=231.
12.) “Microscope Lens.” Pexels, Public Domain Pictures, www.pexels.com/photo/background-binoculars-black-blue-267596/.
13.) Ledford, Heidi. “Alternative CRISPR System Could Improve Genome Editing.” Nature News, Nature Publishing Group, 25 Sept. 2015, www.nature.com/news/alternative-crispr-system-could-improve-genome-editing-1.18432.
14.) Zhang, Chengcheng, et al. “Powerful Technique for Multiplying Adult Stem Cells May Aid Therapies.” Whitehead Institute, Whitehead Institute/ Massachusetts Institute of Technology, 23 Jan. 2006, wi.mit.edu/news/archive/2006/powerful-technique-multiplying-adult-stem-cells-may-aid-therapies.
15.) Toledo, Chelsea, and Kirstie Saltsman. “Genetics by the Numbers - Inside Life Science Series.” National Institute of General Medical Sciences, U.S. Department of Health and Human Services, 11 June 2012, publications.nigms.nih.gov/insidelifescience/genetics-numbers.html.


Congratulations @joelhovell! You received a personal award!
You can view your badges on your Steem Board and compare to others on the Steem Ranking
Vote for @Steemitboard as a witness to get one more award and increased upvotes!