Obstructive Sleep Apnea – quite an ordeal!
In my previous article, I discussed some Surprising Reasons Why Office Jobs Can be Boring.
In that article, I focused on genetics and human nature as some reasons why many people are not really comfortable working common office jobs. In the last part, I mentioned some underlying medical problems like diabetes and sleep apnea.
Let's now focus on obstructive sleep apnea.
[Mask Fitting Prior to Sleep Study]
Why is it important to discuss?
It can be particularly hard to tolerate for students and people who remain seated in their jobs.
If you know someone who snores and feels frequently fatigued or sleepy during the day, please continue reading and share this article with them.
Sleep apnea can cause brain damage and impair memory.
Breathing problems during sleep can cause oxygen deprivation and can possibly hurt the brain as explained in this article: Sleep Apnea May Damage Brain Cells Associated With Memory
This condition remains largely unknown and undiagnosed, especially in our country.
Doctors rarely recommend a sleep study for fatigue. Some symptoms like large tonsils and daytime sleepiness are often either being ignored or treated in isolation. Therefore, it's very hard to see the "big picture".
In the Philippine culture, daytime sleepiness is usually seen as mere "laziness" or boredom. Snoring, which is the hallmark symptom of sleep apnea, is believed to be a sign of "deep/restful sleep" which turned out to be the opposite!
The ambiguous symptoms:
If you usually feel like you're sleep-deprived, even when getting about 8 hours of sleep, there must be a problem somewhere. I won't go into much hard data and technicalities, but I will briefly discuss my own experience and why I think it's really important to consult a doctor about this.
I had a terrible time staying focused at school.
I'd either doze off or zone out during lectures. It seemed like my energy was totally drained after the first class. Aside from excessive daydreaming and lack of energy, I also remember being inconsistent with my performance at school. I would ace some exams and suddenly become bored and sleepy the following day. I'd get the highest grades in some lessons and almost fail other subjects. This selective focusing puzzled my teachers when I was in grade school.
I had mild asthma when I was about 12.
I remember the wheezing sounds I made when breathing. It didn't seem to be life-threatening because I could still breathe with little effort. My mom would accompany me to our trusted pediatrician regularly. Our doctor visits often included a few minutes using a nebulizer. I'd suffer from the intermittent clogged nose (with or without a cough or cold) almost daily. Nobody told us that these conditions could interrupt my breathing and affect the quality of sleep.
I also suffered from frequent tonsillitis until adulthood.
I used to take over-the-counter medicine or home remedies, as a visit to the doctor would almost always mean another visit to the pharmacy for expensive antibiotics. In January 2017, I was also prescribed some antihistamine which didn't seem to help. Again, nobody told me that dry mouth in the morning due to a clogged nose and mouth-breathing while sleeping, causes tonsillitis. Those large tonsils and/or a large adenoid can cause or worsen sleep apnea in a vicious cycle.
Putting all the pieces together:
I never thought that these problems may have been sleep-related! I was looking for solutions for caffeine dependency when I came across sleep apnea. After a few years of searching for answers and multiple doctor visits, I finally figured out that if you snore, you're a candidate for a sleep study. It couldn't be simpler!
Here are some parts of the results of my sleep study done in March 2017: 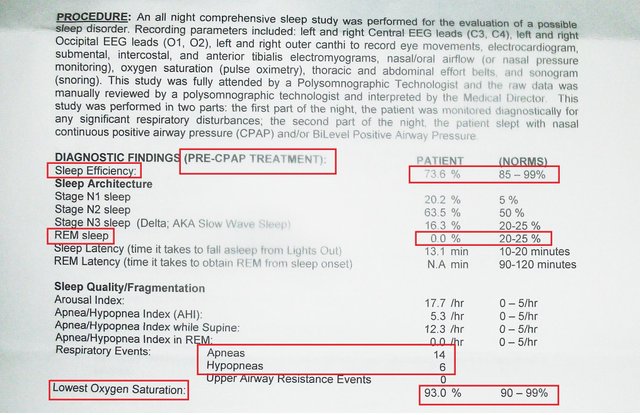
As shown, I've been suffering from mild obstructive sleep apnea. During the split night-study, my breathing was interrupted by about 14 times an hour without a using CPAP. The numbers improved dramatically upon starting treatment!
Before I got diagnosed, I had tried some remedies like a chinstrap and silicone mouthguard. -These apparently helped open my airway just a tiny little bit (but with inconsistent results).
Using a CPAP (Continuous Positive Airway Pressure) machine is by far the best solution for me.

[Actual Unboxing Photographed]
The best treatment, machine settings and results depend from person-to-person, so please avoid self-medication.
I started using CPAP on July 14, 2017, four months after the sleep study. Although CPAP machines are really expensive...
Here are some Good News!
PhilHealth covered my sleep study.
If you have the right medical insurance, you'll probably get covered too! Just look for an accredited hospital with sleep clinics and contact them.
Only a few days into CPAP treatment, I started feeling more active and alert. It's so much better to feel sleepy at night, after having done a lot of work, compared to the mid-morning slump I used to experience everyday.
Your overall health will improve soon after beginning the right treatment as explained in this video:
Brain damage caused by severe sleep apnea is reversible as explained in this article:
Brain Damage Caused by Severe Sleep Apnea is Reversible
There is a new treatment option which is discussed in this video:
Thanks be to God for being there to listen and for all the help I got from my loved ones. If you think you have symptoms of sleep apnea, don't hesitate to seek diagnosis and treatment. Turning to comfort food, smoking, or drinking eight cups of coffee a day may comfort you for a bit without addressing (even worsening) the root of the problem. To those who drink alcohol, please be informed that alcohol is known to relax the airway and make it more prone to get blocked during sleep.
Working night shifts (e.g. at call centers) with the untreated condition may be too much to handle.
If you like to read more about the basics of OSA, please open the link below.
Source: TheFreeDictionary
The cumulative effect of recurrent spells of apnea is hypoxemia and shallow, nonrefreshing sleep, which may lead to excessive daytime drowsiness, personality change, impairment of intellectual function, and heightened possibility of accidents. Obesity, hypothyroidism, cigarette smoking, alcohol, and some hypnotics (particularly benzodiazepines) predispose to OSA, and its prevalence increases with advancing age. About 35% of people with congestive heart failure and 50% of people with hypertension have this disorder, and 50% of those with this disorder have hypertension.
Source: TheFreeDictionary
I've seen SpO2 desaturation of around 60% during severe episodes, the brain detects the change in O2 & CO2 concentrations and rouses the body from sleep for the signature momentary gasping events. So it's quite unlikely that a person would suffocate because your brain and body don't won't to die so they react to prevent it, even when you're unconscious.
Far greater concern is the CO2 accumulation that can occur due to hypoventilation (reduced exchange of gasses via inspiration/expiration).
As CO2 concentration increases so too does the acidity of the blood and other body fluids. While awake there is always the opportunity for deliberate intervention by breathing deeper or faster, but while asleep the process is more of a mechanical homeostatic one with intervention only when certain critical thresholds are crossed. The gasping episodes provide only a brief reprieve from the accumulation, the balance in Ph changes to varying degrees but soon after the trend returns, and the cycle repeats. This can eventually lead to tissue damage, particularly heart muscle among other things. It can also contribute to fatigue, stomach issues, headaches, diabetes, and has impact on Ghrelin and Leptin, two hormones that help regulate metabolism (meta analysis here). This can be a particularly cruel blow to those for whom body mass is a contributing factor to their AHI as the fatigue and metabolic factors compound each other, making it all the harder to reverse.
It's worth pointing out the CPAP & BPAP typically don't supply Oxygen without specific coexisting conditions, these devices simply compress air from the room in which they're operated and deliver it to the user to 'inflate' the soft tissues of the upper airways, mitigating some of the obstruction. Any loss of pressure, such as through the nose or mouth, will reduce the effectiveness.
It's good of you to share this personal experience and insight with others, and to not only point out that diagnosis and intervention may be partially or fully funded under a regional health scheme, but also the contributing factors. The reason I say this is: too many times I've seen an individuals energy and outlook improved by CPAP or BPAP, only to watch them commit with renewed enthusiasm the behaviours that contributed significantly to their condition.
For some conditions CPAP/BPAP are a lifelong association, but for most they are a bridge, an intervention tool, something to give one the best shot at getting stronger and healthier. The other main ingredient, like with many things, is ones self.
You seem very motivated, you'll do quite well.
Thanks for the info brother, hoping and praying for your recovery on your condition.
I didn't even know there was like sleep diagnosis. Please read my last post, it is important. Please state sources for pictures and credit appropriately especially for pictures not owned by you. I left tips for free to use images in my last post
Thank you so much! You provide lots of essential information for Steemians. I can't wait to get a DSLR so I can provide more quality photos.
You are welcome