Chemotherapy ‘Useless’ And ‘Harmful’ For Breast Cancer Patients, Study Finds
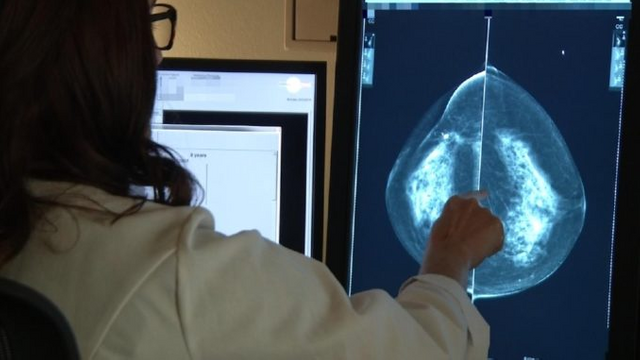
Breast cancer patients who undergo chemotherapy are putting themselves in unnecessary danger, according to a landmark study.
Researchers estimate that over 123,000 women in the U.S. and 23,000 in the UK are subjected to harsh and potentially lethal chemotherapy treatments when they could be treated with new “precision medicine” instead.
Thegaurdian.com reports: “Practically speaking, this means that thousands of women will be able to avoid chemotherapy, with all of its side effects, while still achieving excellent long-term outcomes,” said Dr Harold Burstein, an associate professor at Harvard Medical School.
Breast cancer is the most common cancer in women worldwide. This study looked at women with early hormone-receptor-positive, HER2-negative, axillary-node-negative breast cancer, which accounts for about half of all cases.
For most women, standard care involves chemotherapy and endocrine therapy, in part because of chemotherapy’s proportionally greater benefits for young women.
Chemotherapy is often accompanied by nausea, vomiting, hair loss and fatigue in the short-term, and in rare cases by leukaemia. Researchers were able to separate, through genetic testing, women more likely to have recurrent cancer, which could potentially spare thousands from the treatment.
The study, Trial Assigning Individualised Options for Treatment (Tailorx) was presented as a plenary session at the annual meeting of the American Society of Clinical Oncology in Chicago.
“By stratifying these breast cancer patients and finding that only those with the highest risk of recurrence need to have chemotherapy based on their tumour genetics, Tailorx shows great potential to ensure more gentle treatment without compromising its effectiveness,” said Prof Arnie Purushotham, a senior clinical adviser at Cancer Research UK.
Researchers looked at more than 10,000 women aged 18 to 75. Each had oncotype DX, a type of biopsy that looks at 21 tumour genes. The test assigned women a score from 0 to 100 based on the likelihood cancer would return within 10 years.
Researchers already knew women with scores of 0-10 did not benefit from chemotherapy – about 17% of the women in the study. Conversely, women with a risk score of 26 or more (14% of the study) did benefit from chemotherapy. The study’s aim was to assess the majority of women in the middle, with a score of 11-25.
Of the 10,273 women tested, 6,711 (69%) had a score of 11-25. They were randomly assigned to receive endocrine therapy alone, or a combination of endocrine and chemotherapy. Researchers concluded that, depending on a patient’s age, women who received only endocrine therapy did not fare worse than those who were also treated with chemotherapy.
It means women over 50 with this type of cancer and a score of 0-25 do not need chemotherapy. Women younger than 50 with a score of 0-15 can also avoid the difficult treatment.
The authors said it was the largest precision medicine trial ever done. “It’s fantastic news that this landmark study could now enable thousands more breast cancer patients over 50 to be safely spared gruelling chemotherapy,” said Delyth Morgan, the chief executive at Breast Cancer Now.
“This is another significant step towards personalised breast cancer treatment and we hope these practice-changing findings will now help refine our use of chemotherapy on the NHS.”
“Half of all breast cancers are hormone receptor-positive, HER2-negative, and axillary node-negative,” said the lead author, Dr Joseph Sparano, an associate director of clinical research at Albert Einstein Cancer Center and Montefiore Health System in New York, and vice-chair of the Eastern Cooperative Oncology Group.
“Our study shows that chemotherapy may be avoided in about 70% of these women when its use is guided by the test, thus limiting chemotherapy to the 30% who we can predict will benefit from it.”
Providing chemotherapy costs the NHS about £4,500 for each patient. In the US, chemotherapy can cost more than $140,000 (£105,000). The list price of oncotype DX is £2,580; however, the NHS gets a subsidised rate. Most American insurance companies cover the cost of the test.