This Is Your Brain On Anxiety
Clinical anxiety is a complex disorder; anxious individuals exhibit excessive feelings of unease and apprehension. These feelings may even lead to disabling panic attacks.
A large body of evidence suggests that imbalances of chemical messengers (called neurotransmitters) in your brain and body contributes to anxiety disorders.[1]
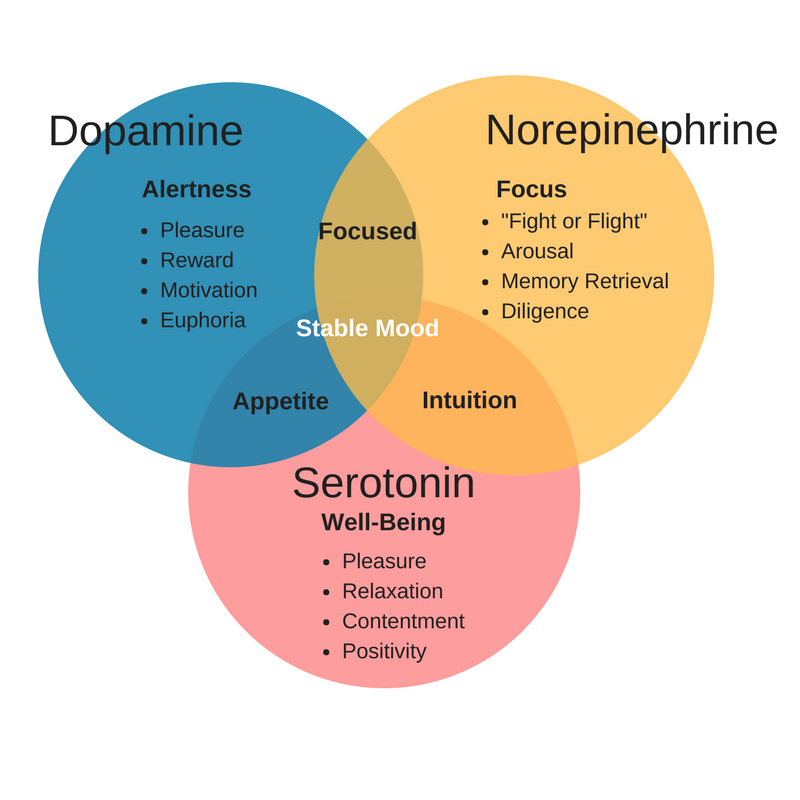
The primary neurotransmitters of concern in anxiety disorders are serotonin, gamma-aminobutyric acid (GABA), dopamine, glutamate, and epinephrine/adrenaline.
The former two are inhibitory neurotransmitters, while the latter three are excitatory neurotransmitters. You will learn about the differences between these two classes of neurotransmitters herein.
This article will take a look at the relationship between your brain, neurotransmitters, and anxiety disorders. You will also learn how gut health can impact neurotransmitter balance and, thus, anxiety. Note that neuropeptides and hormones also play a role in anxiety disorders.
However, those are not the main focus of this article as they differ in mechanisms from neurotransmitters.
The Brain and Anxiety
Anxiety disorders are chronic, debilitating health conditions that inflict major monetary and well-being costs on individuals (and society). In the United States, anxiety disorders are the most common diagnoses in psychiatric practices.[2]
Moreover, a recent 3-year study analyzing over 30 European countries, including 514 million people, shows that anxiety disorders are the most widespread among all other psychiatric conditions.[3]
The current understanding of the mechanisms underlying the pathological forms of anxiety reflects their complexity. That is to say that much of the basis for what causes anxiety is not well understood. However, certain generalities can be made regarding the physiological basis for anxiety.
These generalities derive from studies investigating the processing of negative emotions using different tasks in humans and animals.
An example of such a study is showing anxious patients a series of evoking pictures and assessing the responses in their brain by imaging and/or blood tests for certain chemicals.
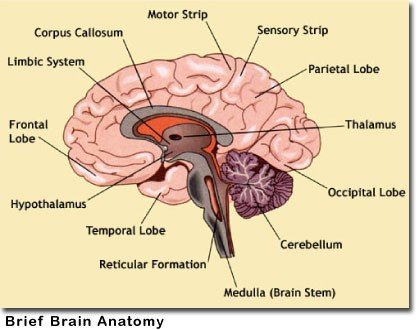
Several brain regions are known to modulate feelings of anxiety and responses to threat/fear, including the amygdala, hippocampus, and prefrontal cortex.
The hypothalamus, midbrain, and even the brainstem are also implicated in anxiety disorders. Overall, these findings suggest that the disruptions in the neurons (nerve cells) and circuitry in your brain form the basis for anxiety.
Distinct neural patterns are continually being tied with states of fear as opposed to anxiety. It is imperative for your brain to be able to make the distinction between fear-specific and anxiety-specific responses.
Per example, if you’re out for a walk and see someone running after you with a weapon, neurotransmitters in your body should trigger an immediate fight-or-flight response; once you escape the imminent danger, the fear-inducing cue goes away (for the most part).
On the contrary, anxiety-specific responses generally arise from threats/cues that are uncertain and not immediate concerns. As such, anxiety lasts longer than fear.
However, scientists propose that there are subjective differences between humans that distinguish fear from anxiety. A large part of these distinctions come from childhood upbringing.
One goal of current research is to comprehend how neurotransmitter, biochemical, and brain circuitry patterns can be clinical predictors of impending anxiety disorders.
Growing evidence suggests that something has gone awry neurologically in children who face excessive adversity growing up; essentially, their brain is under-activated or over-activated in response to stressors.[4]
To this day, studies continually look for ways to predict the likelihood of anxiety disorders utilizing images of the brain. For example, magnetic resonance imaging (MRI) of your brain can detect blood-oxygen levels in specific regions.
Researchers could present you with a series of threatening cues to assess how your brain responds biochemically. Progress is being made, so as time goes on we will learn more about the basis for both fear and anxiety.
Neurotransmitters and Anxiety
In general, certain neurons in your central nervous system (CNS) release neurotransmitters that excite other neurons (meaning they prompt action potentials), while others inhibit (prevent) the creation of action potentials.
These two types of neurotransmitters are known as excitatory neurotransmitters and inhibitory neurotransmitters, respectively.
An action potential is the biological process by which a cell broadcasts a signal to other cells.
For example, in muscle cells, an action potential is the first step in the chain of events leading up to contraction. In neurons, action potentials are influenced by neurotransmitters.
In simpler terms, let’s say hypothetically there’s a neuron in your brain that determines whether you buy a car or not. Let’s also imagine it’s an interneuron, which is involved with cognition and decision making.
Now, pretend a salesman walks up to you at the car dealership with an amazing deal on a Lamborghini; odds are, your brain is going to tell you, “Yes, I want this car!” This thought is going to be pushing the action potential of your neuron to the brink of buying the car.
However, a second thought comes to mind and you think maybe you shouldn’t because your current car works just fine and you want to save your money.
Yet, here you are and the Lamborghini’s headlights are staring you down, telling you to give in to its shiny beauty; now you want the car again. What do you do? There’s impulses telling you that you should and shouldn’t buy the car.
In short, the nervous system’s role in decision making works much like having the devil on one shoulder, telling you to give in, and an angel on the other telling you to resist temptation. The former is essentially an excitatory neurotransmitter and the latter is an inhibitory one.
The following sections take a deeper look at how these neurotransmitters work and their role in anxiety.
Inhibitory Neurotransmitters
Serotonin (5-Hydroxytryptamine)
Serotonin, also known as 5-HT, is a monoamine neurotransmitter made from the amino acid L-tryptophan.

Serotonin is often touted as the “feel-good” neurotransmitter, but that might be a bit of a misappropriation as other neurotransmitters are known to increase pleasurable feelings.
Over 90% of your body’s total serotonin content is in the gastrointestinal tract, where is helps stimulate the intestines. The remaining ~10% of serotonin content in your body is made in the CNS by serotonergic neurons.
Serotonin acts throughout your brain to regulate mood, appetite, sleep, and cognition. After serotonin completes its actions, it is recycled back into neurons by a protein called serotonin transporter (SERT).
If you’re familiar with selective serotonin-reuptake inhibitors (SSRIs), chances are you know that they work by blocking the actions of SERT proteins.
The serotonin system has long been implicated in the mediation of anxiety. For example, genetic variations in the human SERT protein and in certain serotonin receptors influences anxiety traits.
Moreover, mice who lack the genes that encode for (i.e. create) serotonin receptors show increases in anxiety-related behavior. Even more, drugs that block serotonin receptors restore anxious behavior.
Not surprisingly, if your brain doesn’t use serotonin efficiently, or levels are low altogether, anxiety and depression are more likely. Thus, serotonin is currently a primary target of anxiolytic medications.
SSRIs are the most common prescription drugs for clinical depression and anxiety. Other medications, such as buspirone, target specific serotonin receptors in your brain and enhance the effects of the neurotransmitter.
Promisingly, a good amount of literature shows that natural remedies are just as viable for serotonin malfunctions. Nootropics such as 5-hydroxytryptophan ( - a precursor to serotonin - readily passes into the brain and increases serotonin levels.[5]
Other nootropics, such as inositol, appear to restore serotonin receptor functions.[6]
On a final note, too much serotonin is not inherently a good thing either. Serotonin syndrome is a potentially fatal condition in which your brain produces too much serotonin.
Symptoms of this condition typically include agitation, rapid heartbeat, hallucinations, and loss of coordination. In fact, illicit drugs, such as LSD and ecstasy, are common causes of serotonin syndrome. Like with most all chemicals, the difference between medicine and poison is in the dose.
Gamma-aminobutyric acid (GABA)
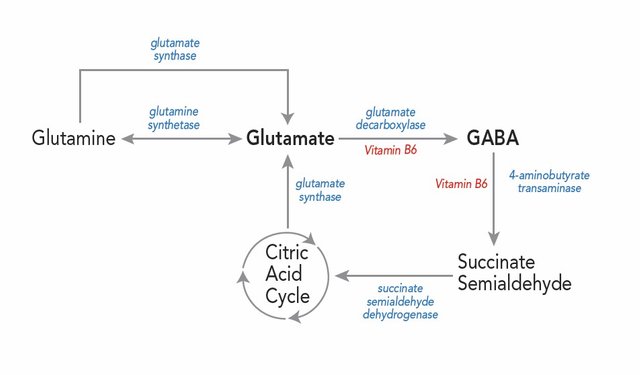
GABA is the main inhibitory neurotransmitter in the CNS. It is created exclusively within neurons from glutamate and then degraded to succinate (which is sent to the Krebs cycle for energy production).
It’s pretty amazing that the principal excitatory neurotransmitter, glutamate, can be converted to GABA (the principal inhibitory neurotransmitter) in a single step (see diagram below); it just goes to show how delicate your brain and body really are.
Dysfunction in GABAergic neurotransmission appears to play a large role in anxious behavior.[7] In fact, more than 30% of all neurons in the central nervous system use GABA to transmit signals to one another. Lack of GABA in the CNS can even produce convulsions and feelings of mania.
Research demonstrates that GABA acts primarily to block the production of excitatory neurotransmitters, such as glutamate; thus, when GABA levels increase, you are more likely to feel calm and restful.[8]
Naturally, you might assume that glutamate is inherently bad for anxiety purposes. However, glutamate is the very compound that your body needs to create GABA.
Enzymes in your nervous system have interplay among one another to keep a balance between GABA and glutamate. Certain drugs exist that either enhance or block the activity of the enzyme glutamic acid decarboxylase (GAD), which is what enables glutamate to be converted to GABA.
Furthermore, a variety of GABA-based anxiety reducing drugs exist, particularly compounds called benzodiazepines. These drugs readily activate GABA receptors and enhance their effects. Certain over-the-counter nootropics can mimic the effects of these drugs, such as phenibut and even GABA itself.
Excitatory Neurotransmitters
Adrenaline (Epinephrine)
Earlier in this article we alluded to a “fight-or-flight” response to fear; adrenaline is the neurotransmitter (and hormone) that tells you to either start running for your life or stand your ground. Adrenaline is a catecholamine made from noradrenaline (which comes from dopamine).
Adrenaline is technically a stress hormone, but is vital for longevity. Note that stress is not always a bad thing; in fact, adrenaline boosts mental alertness and feelings of pleasure.
It’s much like a good form of stress, one that makes you feel more alive and perceptive. Therefore, producing adequate amounts of adrenaline is key for making you feel better and keeping you active.
On the same token, too much adrenaline can elevate heart rate and disrupt your ability to calm down; obviously, that will make anxiety worse. In fact, people who pass out and can’t be revived through CPR may be given an injection of adrenaline; this will almost instantly get their heart pumping rapidly again.
are the two most common nootropic ingredients to boost adrenaline. Generally, using these ingredients earlier in the day is best to make sure they don’t cause any sleep loss.
Dopamine
Dopamine is made from the amino acid L-tyrosine and serves as an ever-present excitatory neurotransmitter that pervades both the central and peripheral nervous systems.
It is a common target of treatment in motor control disorders, such as Parkinson’s disease, and seizures, as it controls muscular tone. Dopamine is also crucial for mental focus and reducing anxiety, particularly by promoting feelings of motivation.
Dopamine is the instigator in your brain when you feel the motivation to accomplish something because of an impending reward. For example, if you’re really hungry for pizza, dopamine levels rise as you scarf down each slice and satiation increases.
However, if you eat the entire pizza, you may suffer from dopamine withdrawal shortly after as the “high” quickly heads south.
Naturally, addictive substances, like cocaine and even sugar, often act on dopamine levels in your brain. In fact, cocaine and sugar exhibit nearly identical stimulation of the brain (which is unnerving, to say the least).[9]
Nevertheless, dopamine can be a great neurotransmitter for relieving anxiety; of particular note is that it reduces cortisol production, which is the main stress hormone in the body.[10] High cortisol levels are a commonality among people who have panic attacks.[11]
Dopamine also appears to stimulate growth hormone release, and vice versa. This is a positive because as you age, a decline in dopamine signaling occurs. Research shows that growth hormone can counteract this decline, and in turn, restore cognitive function.[12]
The most effective way to increase dopamine levels naturally is use of the nootropic L-DOPA.
Glutamate
Glutamate is the main excitatory neurotransmitter in the central nervous system. As touched on in the GABA section, it is made from the Krebs cycle and from the amino acid L-glutamine (which is the most abundant amino acid in your body).
Glutamate levels tend to be too high in individuals with anxiety. Thus, anxiolytic drugs that target glutamate typically block/reduce its creation.
Unfortunately, the chemicals that do this tend to be toxic even in small amounts.
As it stands, the most efficacious way of reducing glutamate production, is increasing GABA levels.
The Gut Microbiome and Neurotransmission
The human gut contains upwards of three pounds of bacteria – made up of over 1000 different species - that help you digest and absorb nutrients from food.[13] These microbes are jointly referred to as your gut microbiome.
A healthy gut microbiome is essential for hormone production, immune function, and even body-weight regulation.[14],[15],[16]
Research in recent years also highlights that microbes in your gut may also influence neurotransmitter production.[17] This connection is known as the brain-gut axis.
The mechanisms behind this connection require further research, but appear to come from the ability of gut microbes to control tryptophan metabolism.
As you age, lack of stability in the gut may lead to decreases in serotonin synthesis and increase production of harmful chemicals.
While most people fear bacteria and living things not visible to naked eye, these microscopic life forms can actually benefit (or harm) you in many ways, it’s just a matter of nourishing the right species.
Lactobacilli and bifidobacteria appear to be the two most beneficial species at this time.[18] But how do you promote the growth of these bacteria? Read on as we explain.
How to Improve Gut Health
Due to the emerging evidence of gut microbiome importance, supplement companies that manufacture probiotics are seeing sales sky rocket. Probiotics are usually a capsule form of live bacterial cells that are thought to promote better gut health.
Research shows the emerging efficacy of probiotics and a healthy gut microbiome, which in turn has implications for treating anxiety naturally.
In past decades, a major hindrance for probiotics was finding bacteria that could survive the acidic environment of your stomach. Stomach acid is low in pH (i.e. highly acidic) and readily destroys/breaks down many substances, as well as living things such as bacteria.
Thankfully though, advances in biotechnology make modern-day probiotic supplements much more viable thanks to bacterial strains that readily survive in your stomach.
Furthermore, the gut microbiome feeds on undigested fiber and prebiotics; by eating a diet rich in soluble fiber, insoluble fiber, and special types of carbohydrates such as resistant starch and fructooligosaccharides, you give healthy bacteria the nutrients they need to flourish.
These types of carbohydrates are typically found in foods like sweet potatoes, bananas, tapioca, and artichoke.
Take-Home Points
Anxiety is driven by dysfunction in neural circuitry and neurotransmitter imbalance(s).
The cause of these dysfunctions appear to be environmentally and genetically driven.
Anxiety disorders are the most common diagnoses among all psychiatric conditions in many countries.
Fear is distinct from anxiety, but there’s a subjective difference between humans as to what constitutes an imminent threat.
In general, fear arises from an immediate cue of danger; anxiety is long-term apprehension in the absence of certain threats/cues.
Neurotransmitters are either inhibitory or excitatory; the former increase the likelihood of action potentials while the latter decrease the likelihood of actions potentials.
Action potentials are ultimately what determine what you do and what you don’t do.
Serotonin and GABA are inhibitory neurotransmitters that promote calmness and relaxation.
Dopamine, glutamate, and adrenaline are excitatory neurotransmitters that elevate heart rate, mood, and cognition.
The human gut contains over 1000 species of microbes, and plays an important role overall health and serotonin production.
Eating a healthy diet is key for stimulating growth of the right bacteria and starving bad bacteria.
References:
[1] Shri, R. (2010). Anxiety: causes and management. International Journal of Behavioral Science (IJBS), 5(1).
[2] Kessler, R. C., Petukhova, M., Sampson, N. A., Zaslavsky, A. M., & Wittchen, H. U. (2012). Twelve‐month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International journal of methods in psychiatric research, 21(3), 169-184.
[3] Lieb, R., Becker, E., & Altamura, C. (2005). The epidemiology of generalized anxiety disorder in Europe. European Neuropsychopharmacology, 15(4), 445-452.
[4] Woodward, L. J., & Fergusson, D. M. (2001). Life course outcomes of young people with anxiety disorders in adolescence. Journal of the American Academy of Child & Adolescent Psychiatry, 40(9), 1086-1093.
[5] Birdsall, T. C. (1998). 5-Hydroxytryptophan: a clinically-effective serotonin precursor. Alternative medicine review: a journal of clinical therapeutic, 3(4), 271-280.
[6] Fux, M., Levine, J., Aviv, A., & Belmaker, R. H. (1996). Inositol treatment of obsessive-compulsive disorder. The American journal of psychiatry, 153(9), 1219.
[7] Nemeroff, C. B. (2002). The role of GABA in the pathophysiology and treatment of anxiety disorders. Psychopharmacology bulletin, 37(4), 133-146.
[8] Lydiard, R. B. (2002). The role of GABA in anxiety disorders. The Journal of clinical psychiatry, 64, 21-27.
[9] Avena, N. M., Rada, P., & Hoebel, B. G. (2008). Evidence for sugar addiction: behavioral and neurochemical effects of intermittent, excessive sugar intake. Neuroscience & Biobehavioral Reviews, 32(1), 20-39.
[10] Oswald, L. M., Wong, D. F., McCaul, M., Zhou, Y., Kuwabara, H., Choi, L., ... & Wand, G. S. (2005). Relationships among ventral striatal dopamine release, cortisol secretion, and subjective responses to amphetamine. Neuropsychopharmacology, 30(4), 821-832.
[11] Charney, D. S., Woods, S. W., Goodman, W. K., & Heninger, G. R. (1987). Neurobiological mechanisms of panic anxiety: biochemical and behavioral correlates of yohimbine-induced panic attacks. The American journal of psychiatry.
[12] Shuto, Y., Shibasaki, T., Otagiri, A., Kuriyama, H., Ohata, H., Tamura, H., ... & Wakabayashi, I. (2002). Hypothalamic growth hormone secretagogue receptor regulates growth hormone secretion, feeding, and adiposity. The Journal of clinical investigation, 109(11), 1429-1436.
[13] Sears, Cynthia L. (2005). A dynamic partnership: Celebrating our gut flora. Anaerobe. 11 (5): 247–51.
[14] Turnbaugh, P. J., & Gordon, J. I. (2009). The core gut microbiome, energy balance and obesity. The Journal of physiology, 587(17), 4153-4158.
[15] Evans, J. M., Morris, L. S., & Marchesi, J. R. (2013). The gut microbiome: the role of a virtual organ in the endocrinology of the host. Journal of Endocrinology, 218(3), R37-R47.
[16] Kau, A. L., Ahern, P. P., Griffin, N. W., Goodman, A. L., & Gordon, J. I. (2011). Human nutrition, the gut microbiome and the immune system. Nature, 474(7351), 327-336.
[17] O’Mahony, S. M., Clarke, G., Borre, Y. E., Dinan, T. G., & Cryan, J. F. (2015). Serotonin, tryptophan metabolism and the brain-gut-microbiome axis. Behavioural brain research, 277, 32-48.
[18] F. Ozogul, E. Kuley, Y. Ozogul, I. Ozogul. (2012). The function of lactic acid bacteria on biogenic amines production by food-borne pathogens in arginine decarboxylase broth. Food Sci Technol Res, 18, pp. 795–804
Thanks for the good article