CONTEST ENTRY: It's All Greek-Science-Geek To Me, Cryptorchidism

To enter @ruth-girls 's Greek-Science-Geek contest I am extending on the topic of my previous post and covering the term cryptorchidism.
Although the first part of this compound word is shared with the term cryptocurrency and might sound like an ICO for a crypto token for the cultivation and breeding of orchids, it is not blockchain related.
Let's first listen to how this word sounds in English and Greek spoken by a non-native English and a non-Greek speaker, such as me:
To depict the term, I decided to use a volunteer model. Due to the unavailability of the model for a second trial of photos, I had to redraw the writing with a photo editor to make it more visible.

Cryptorchidism = κρυψορχία,
fromκρυφός (Latin spelling: kryptos) – hidden
and
όρχις (Latin spelling: orchis) – testicle,
is not the reluctance of male individuals to expose their bollocks, as you might have figured from the picture.
Cryptorchidism is a term defining a medical condition (ICD-10 code Q53) characterized by the failure of one or both of the male testis to locate to their physiological position in the scrotum during fetal and early neonatal development. It is synonymous with the term “undescended testis” (UDT). A male infant is considered to have UDT when his testis have not yet descended to the scrotum by six months after birth.
Let's take a more detailed look at what cryptorchidism is and how it arises.
Development of the testis:
The testis develop in the male embryo from the same mass of primordial germ cells that give rise to the ovaries in the female. The site of gonad development locates to both sides of the abdomen along the spine, below the lower poles of the kidneys. The gene of the male-specific Y chromosome called SRY, (sex-determining region of Y chromosome), activates a molecular cascade triggering the yet uncommitted gonads to differentiate into Leydig cells (producing testosterone) and Sertoli cells. Sertoli cells secrete the anti-Muellerian hormone, that inhibits the development of the primordial uterus and fallopian tubes. Sertoli cells later provide the nurturing framework for the spermatagonia to develop into mature sperm cells.
During the mid- and late gestation period the testis first descend from their site of origin to the inguinal channel along a ligamental structure called gubernaculum testis. This movement is assumed to be the consequence of locomotive cues provided by a hormone called relaxin or INSL3 and its receptor RXFP2. In a second step the testis descend from the inguinal channel into their final location in the scrotum, again promoted by gubernaculum testis that itself is thought to be directed by calcitonin gene-related peptide, a hormone originating from neighboring nerves.
During the descent from the abdominal retroperitoneal space (i.e. behind the encapsulated digestive tract organs) to the front of the body, the testis invaginate the peritoneal membrane (the capsule around the intestines). By doing so they wrap themselves and the appending structures, such as the vas deferens, (the cord that transports sperm to the penis during ejaculation), in two layers of serous peritoneal tissue, which becomes designated as the tunica vaginalis. The peritoneal process, that got dragged by the testis through the inguinal channel, gets obliterated later in life, but its remnant, the processus vaginalis, is a culprit that enables the development of inguinal hernia. Given a weakness of the abdominal wall, parts of the intestines can get trapped in this processus and even end up protruding into the scrotum. This is a dangerous situation as it can lead to the incarceration of the affected intestinal segment.
Incidence and diagnostic varieties of cryptorchidism:
An estimated 1% of boys are born with one or two undescended testicles, with Denmark being an exception and reporting about 9% of boys born with this defect.
The testis can get stuck anywhere on their physiological path of descent: in the abdomen, in the inguinal channel, or short of getting settled deep in the scrotal sack.
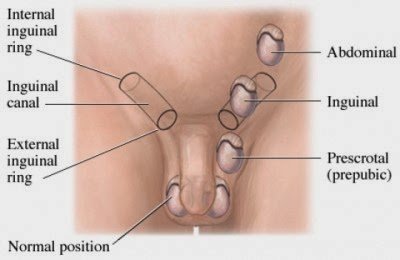
In rare cases, the testis can even deviate from its path and divert to ectopic sites in the groin and pubis.
A diagnostic distinction is made between palpable and non-palpable cases. Palpable testis can be found by examining the scrotum and inguinal regions with the hands. In case of non-palpable testis, the organ either resides in the abdomen or is atrophied or even absent. Diagnostic procedures include ultrasound, MRI and laparoscopy. When both testis are absent from the scrotal sack, normal hormonal response should be verified to exclude intersex conditions.
Furthermore, some males present with retractile testis, i.e. the testis tend to retract back into the inguinal channel due to a triggered cremaster reflex. This situation is not a true cryptorchidism and usually of benign nature. In contrast, there are cases of ascending testis after birth - an acquired cryptorchidism.
Etiology and risk factors:
Although it is not clear what exactly causes cryptorchidism, it is likely to be the consequence of the disruption of the normal male hormonal response axis. Mutations in the aforementioned genes INSL3 and RFXP2 genes have been associated with cryptorchidism in patients. Cryptorchidism often accompanies conditions such as Klinefelter, Down and Noonan syndrome. It occurs more often in prematurely delivered and low birth infants and from mothers who experienced gestational complications or consumed nicotine during pregnancy. Furthermore, cryptorchidism occurrence is reduced in breastfed and increased in soy formula fed infants. In addition, environmental, hormonally active compounds have been suggested to provoke cryptorchidism although definitive evidence has not been provided yet.
Health consequences of cryptorchidism:
For the execution of its normal function to produce mature sperm cells, the testis requires a working temperature that is below the body core temperature. This is the reason why the testis need to migrate to the exterior of the male body, in contrast to the intraabdominally functioning female ovaries. The persistingly higher than optimal temperature within the abdomen leads to the deterioration and, finally, atrophy of undescended testis. As a consequence, males with a history of bilateral cryptorchidism show a reduced fertility / paternity rate. A unilateral UDT, however, does not seem to significantly impact on reproductive function since the normally developed testicle is unaffected.
Most alarmingly, patients with UDT have an up to three-fold increased risk of developing testicular cancer. In unilateral cryptorchidism, the cancer rate for the normally developed testicle is elevated as well. Reported rates dramatically higher than around 3 might be confounded by the inclusion of patients who have more fundamental underlying pathologies such as the cancer-associated Noonan syndrome. If an undescended testicle is identified post-puberty, it should be removed due to the high risk of it to sprout testicular cancer.
Therapy:
The recommended therapy for cryptorchidism is orchiopexy. In this surgical procedure the undescended testis is revealed at its respective location, prepared and carefully brought back and fixated into the scrotum with its accompanying blood supply and spermatic cord. For illustrative material and not for the faint-hearted readers, please refer to the freely accessible review by Braga & Lorenzo, 2017 or an animated education video.
The procedure should be carried out not later than 12 months after birth since at later timepoints the affected testis already shows signs of degeneration with reduced organ volumes and Sertoli cell numbers and drastically diminished sperm cells numbers.
Awareness:
Primary care providers must be aware of this quite common condition since a delayed diagnosis might render the male patient infertile. Adequacy of primary care is, unfortunately, not always guaranteed. Furthermore, male UDT patients should be educated about their increased testicular cancer risk and taught how to palpate their testis for any irregularities at adulthood.
Parents have to take responsibility for their children and I would like to suggest the 21st of October as the cryptorchidism awareness day. It should be a pointer to parents to examine their infants for correct, scrotal position of the testicles. It should also serve as yet a further reason to act responsibly and cease smoking and drinking during pregnancy!

Picture by aussiegall
Yours, @replichara
References:
1. http://dictionary.cambridge.org/us/dictionary/english/cryptorchidism
2. http://en.bab.la/dictionary/english-greek/cryptorchidism
3. http://www.wordreference.com/gren/κρυφός
4. http://www.wordreference.com/gren/όρχις
5. https://www.omim.org/entry/146738?search=INSL3&highlight=insl3
6. https://www.omim.org/entry/606655
7. Lee PA, Houk CP. Cryptorchidism. Curr Opin Endocrinol Diabetes Obes. 2013 Jun;20(3):210-6.
8. Braga LH, Lorenzo AJ. Cryptorchidism: A practical review for all community healthcare providers. Can Urol Assoc J. 2017 Jan-Feb;11(1-2Suppl1):S26-S32.
9. Shepard CL, Kraft KH. The Nonpalpable Testis: A Narrative Review. J Urol. 2017 Apr 21. pii: S0022-5347(17)54873-9.
10. https://www.mayoclinic.org/diseases-conditions/undescended-testicle/symptoms-causes/syc-20351995