Peripheral Facial Paralysis (PFP)
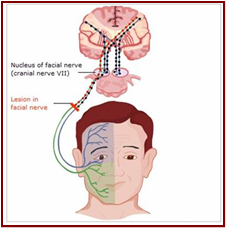
Facial nerves direct the muscles on one side of the face, control the blinking and closing of the eye, as well as the non-verbal expressions of some of our emotions, as well as being responsible for transporting nerve impulses to the lacrimal glands, salivary and muscles of a small bone in the middle of the ear called stirrup, in addition to transmitting sensations of taste coming from the tongue.
Peripheral Facial Paralysis (PFP) occurs when the operation of the facial nerve is interrupted, that is, communication between the brain and the facial nerves is interrupted as shown in the image below.
The Peripheral Facial Paralysis (PFP) not only implies a loss of movement, but also the commitment of an area of broad contact with our environment, as is the face, with the consequent emotional and labor implications.
Facial paralysis is the most frequent paralysis of a peripheral nerve. The vascular anatomical substrate explains its vulnerability, it can be the result of an infection, tumor, vascular or traumatic compression, among other causes.
The most common concern when facing a facial paralysis is to define or determine if it is peripheral or central type. Being peripheral, it must be evaluated in which part of the path the nerve is affected and thus define the patient's prognosis.
Symptoms:
Among the symptoms described by patients with PFP are:
• A lot of burning in the eyes, due to the absence of flicker.
• Excessive lacrimation or dry eye syndrome.
• Difficulty in aspirating or blowing.
• Deviation of the corner of the lip to the opposite side preventing fluid retention.
• Otalgia: symptom that occurs in the outer or middle ear.
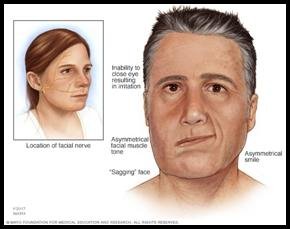
• Alteration of facial expression due to high hemifacial motility.
Signs:
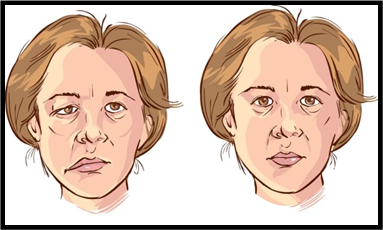
Facial paralysis is diagnosed given the facial asymmetry and can be evidenced:
• Predominance of the muscles of the face on the normal side, pulling the face to the same side.
• Elimination of wrinkles and grooves on the paralyzed side.
• No wrinkles are formed on the forehead, preventing brow furrowing.
• Lagophthalmos: the patient can not close the eye on the paralyzed side.
• Bell sign: when the patient closes the eyes, on the paralyzed side, the eye is directed upwards.
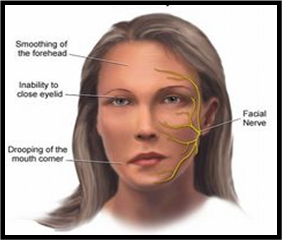
In peripheral facial paralysis, bilateral paralysis may occur, but the one that occurs most frequently is unilateral paralysis, resulting in an inability to frown, close the eyes or show the teeth.
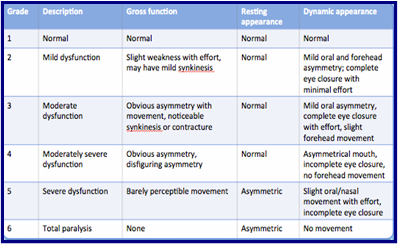
The facial deformity is quantified depending on the degree of injury and the time of onset of paralysis. At present, the House-Brackmann classification is used to quantify facial paralysis. (see table)
Medical treatment:
• The eye area should be protected and thus avoid corneal ulceration, this is achieved with the application of artificial tears, washed with serum and nighttime occlusion.
• Treatment with corticosteroids is necessary, including Deflazacor, Prednisona.
• Use vasodilators, vitamin B complexes, gangliosides, antivirals and antibiotics, among others.
• Perform physical therapy exercises because the paralyzed muscles can shrink and shorten and thus cause permanent contractures.
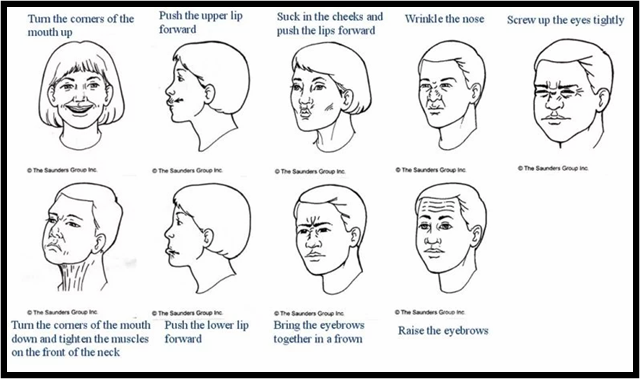
The following image shows some exercises that a patient with facial paralysis should perform: