Mad Lad Scientist Heals Millions
In today´s post I will cover a topic I wanted to write about for such a long time. It has everything I find intriguing in a good story: an unsolved mystery, unknown danger, a daring hero and a well-deserved reward and happy ending. This story led to the discovery of a cure for one of the most frequent health problems in the Western world. However, as is often the case in science, the answer is never totally right, and recent research shows that conclusions may have to be changed a little bit. Anyways, without further delay, enter stage: Barry J. Marshall.
Barry Marsall is an Australian doctor who was born in 1951 and who grew up in Perth, Australia. He recalls reading his dad´s technical books, but most importantly, his mum´s nursing books in his childhood. His interest in medicine was further strengthened when his younger sister accidentally drank kerosine. Young Barry, after calling the ambulance, performed some CPR techniques he learned in swimming class, during which he discovered the smell of kerosine coming out of his sisters mouth - diagnosis: poisoning. After some dangerous experiments as a youth, he had to decide what to study at college: electrical engineering or medicine. Due to his self-perceived weakness in calculus, he decided to study medicine. After he graduated, and starting his family, he began rotating different medical specialities. It was during one of these rotations that he met Robin Warren, who was investigating curved bacteria that were found in patients´ stomach biopsies. He was very intrigued by previously undescribed bacteria, that live in the harsh environment of the stomach. This is where I will pick up and go into more sciency details.
The Issue
The stomach is a vital element in our digestive system. It plays various roles. Food arrives from the mouth in the form of a so called bolus. It is pre-chewed and enriched with the enzyme amylase, which begins the break-down of complex carbohydrates into simpler, absorbable once. The stomach further breaks down the food by contraction of strong muscles. Further specialized cells in the stomach release potent chemical agents. Parietal cells secrete hydrochloric acid (HCl), while the so called chief cells secrete pepsinogen, an enzyme that breaks down proteins. Furthermore, mucous cells secrete an alkaline mucus which protects the stomach from its contents. This lining is essential for the stomach to be healthy. Its alkalinity (pH > 7) protects it from the HCl acid (pH 2-4) protects the stomach cells from taking damage from the acid. It further separated the cells from pepsinogen. Many of the functional units in cells are based on protein, so a protein-digesting enzyme does not go well with protein-heavy cells.
There are many other mechanisms the stomach is involved in, ranging from controlling secretion of the cells I mentioned above, as well as in control of hunger. If you want to learn more about the physiology of the stomach, or physiology in general, I would recommend buying and reading a physiology text book. I am using a book called "Human Physiology: From Cells to Systems" by Lauralee Sherwood (you see, no link here, I do not get paid for mentioning this book). There are probably many other phsyiology books out there and they are likely all good. I just want to challenge you to go and get one for yourself and feed your curiosity!

Anyways, back to the topic. The mucosal layer in our stomach is very reliable, but issues do occur - nothing is ever perfect. There are many possible disturbances, but in the 80s two were of particular interest to Dr. Marshall and Dr. Warren: Gastritis and ulcers. According to Psychyrembel: Klinisches Wörterbuch (clinical vocabulary) and ulcer is simply a sore (ulcer is best described as an ulcer) and gastritis is an infection of the stomach lining. Both can potentially be very dangerous. In most cases patients observe pain in the region of the stomach (this can be very severe pain). In very bad cases, the ulcers can start bleeding (which can become dangerous) and there is also a chance that in very severe cases the lining of the stomach can be broken through by the stomach acid, which is a life-threatening situation. As you can see, stomach ulcers, the main focus of my post (sorry gastritis), should not be taken lightly.
It was very difficult to find reliable data about the occurence of peptic ulcers. Studies done on kids differ widely in their results. One study found that 56 out of 694 children who went to have an upper gastrointestinal endoscopy. This study is not entirely appropriate because it only included children that already were suspected to have some sort of gastric disease and because the study was run for only one month. Another study found that between 1997 and 2000 peptic ulcers occured in 30.35% of studied cases, while between 2007 and 2010 20.19% of cases where found to have peptic ulcers. This study was a meta study. However, the frequency is relatively high and did not really give me the information I was looking for. A review on the topic of stomach ulcers I found stated a study that used population-wide gastro-enteroscopies (sending a little camera down the oesophagus into the stomach), which found a prevalence of 4.1%. I consulted a book I have been using quite a bit these days called "Lehrbuch der Inneren Medizin" by Siegenthaler et al. In chapter 12 "Krankheiten des Verdauungstraktes" (diseases of the digestive tract), they state that roughly 7% of the "working, male population" had stomach ulcers at one point in their life. What about women? And unemployed people? Well, I had to visit organizational websites, like that of the NHS. Here they state that 1 in 10 (so 10%) of people will have a peptic ulcer at some point in their life. Because this seems to be some sort of guessing game, let´s say that 7% of people will have to deal with a stomach ulcer once in their life. I am still not satisfied. And here is why.
Like virtually any health issue (except for maybe a paper cut), peptic ulcers do not have one single cause. For a very long time, people assumed that stomach ulcers are caused by a bad diet and stress. This misconception has been very dominant until the 90s and can still be found today. While scientific studies have shown that diet is not an indipendent risk factor, it is agreed upon that it does pose a risk in combination with an independent risk factor. A review and a study have shown that uptake of certain non-essential nutrients can help in the prevention of stomach ulcer, even though both sources stated that this is not yet proven. Anyways, it appears that a diet rich in fiber, as well as vitamin A and polyphenols can be beneficial. If you want to apply this to your life, do not even dare to buy supplements. You can find all these great things in fruit and vegetable. As I have written in a previous post (Link), it is better to eat fruit as a whole, with a mix of beneficial nutrients. This is due to so called, not well understood, synergistic effects. Meaning that the combination of compounds is a greater factor, than the individual components themselves. This could fill an entire post, so if you are interested, do some work yourself and learn for yourself.
Well, diet not being an independent factor, what about stress? Eventhough the scientific community has moved away from an initially "stress only" theory to a "bacteria only" theory, it is evident that stress still plays a factor in the development of stomach ulcers. Studies have shown that people who classified themselves as stressed, had a higher chance of developing an ulcer. However, this study relied on self-perceived stress which cannot be very objective. Sadly stress cannot yet been quantified reliably. Anyways, instead of seeing stress as an entirely separate risk factor, some scientists voice the theory that stress may play a co-factor role, together with bacteria. You can probably link that to the effects of stress on the immune system. As I have written in my most recent post (Link), stress can downregulate the immune response, thus enhancing the chances of an infectious agent.
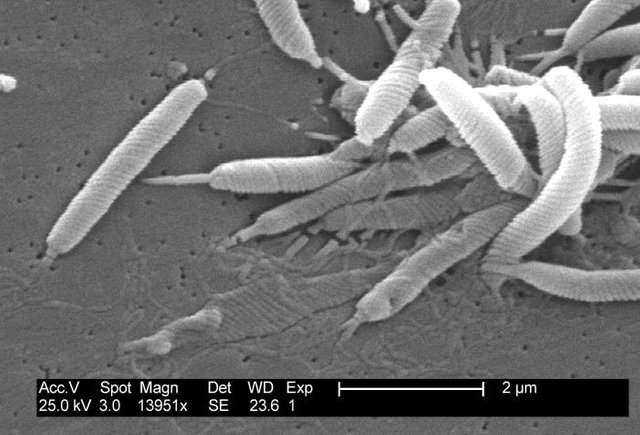
Microbes are easily the most fascinating living things on this planet. We may be smarter, but these things manage to live everywhere: you, your house, glaciers, waters, probably space and your stomach. Whatever you throw at them, they are likely evolve to survive. And H. pylori has evolved to live in our stomach. In our stomach, the bacteria secrete an enzyme (urease), that converts urea into ammonia and carbon dioxide, effectively increasing (de-acidifying) their environment to the point that they can live in the stomach. Propelled by flagella that develop at a pole of the bacteria (only on one side of it) it moves into the mucosal layer of the stomach linen. Here it secretes more enzymes, collagenase and mucinase, which allows H.pylori to break through the mucosal layer and reach the cells that make up the inner lining of the stomach. Here it nestles itself and builds a colony. Bacteria eat, and they secrete waste. Among the secretions of H. pylori are several cytotoxins. Vacuolating cytotoxin and neutrophil activating protein induce apoptosis (programmed cell death) in surrounding cells, leading to tissue damage and a decrease in local immune defense activity. Another big problem is the release of a protein called CagA, which interferes with the host cells´ (our cells) signal transduction. This is a very complicated topic, but in short CagA stimulated cell division and growth. Thus, it may cause cancer.
An Important Collaboration
All of this has not been known until the 80s, when Dr. Marshall and Dr. Warren started to work together. They successfully isolated the weirdly looking bacteria from patients with gastric ulcer. Since Dr. Marshall was still in his training, he had to move to other hospitals, which stalled the progress on the joint project. Once Marshall found a position at a local hospital in Perth, the work continued. By that time Marshall and Warren had gained some support internationally, but also criticism. Dr. Marshall in particular received a lot of criticism and was struggling to get his hypothesis proven. Unable to reproduce his findings in humans with animal studies (alas giving animals H. pylori cultures and seeing if ulcers develop), people said that his conclusions were premature and that the bacteria were contaminants. At that time Dr. Marshall was already treating patients with antibiotics and bismuth, a cheap treatment that could cure ulcers within two weeks without the need of surgery. In order to get his theory accepted by the wider science community he decided to take a drastic step. He used himself as an animal study and drank an H. pylori culture, after getting a baseline endoscopy done. While he already assumed that he would get an ulcer, he was surprised by how well these results supported his theory. Now that he had shown that H. pylori could cause ulcers, he had to treat himself with antibiotics. Dr. Marshall overcame the infection and soon got funding to perform a double-blind study to investigate whether antibiotics were able to cure stomach ulcers. Although it still took time for his theory to be accepted, the cure for a vast amount of stomach ulcers was found. Dr. Marshall and Dr. Warren were both awarded a Nobel prize in 2005.
Nuke H. Pylori!

Yes, they can cause stomach ulcers, gastritis and possibly cancer BUT more than often do not. It is estimated that H. pylori is present in more than 50% of the world´s population. Thus, do not take antibiotics unless you actually have an ulcer and are adviced by a doctor to do so. Because antibiotics have side-effects, not just on the individual but also the population and the environment, preventative treatment of H. pylori is not being done. There is talk of a vaccine, but the development proves to be dangerous. Additionally, H. pylori does have benefits. It seems like it plays a preventative role in several diseases including acid reflux (GERD), Barrett's esophagus and esophageal adenocarcinoma. There is also talk that not merely the presence of H. pylori causes ulcers, but rather a disturbed "equilibrium" between the bacteria and the host. This theory is supported by the fact that H. pylori colonization in humans is decreasing, while the occurance of gastric ulcers was on the rise. Studies also suggest that H. pylori is protective against diseases of the oesophagus. Thus, getting rid of H. pylori could cause harm, and not just benefits. Nuking all H. pylori with antibiotics, as well as the notion "only a dead H. pylori is a good H. pylori", should be reconsidered as more evidence for potential H. pylori benefits arise. There is another big risk factor for stomach ulcers, which takes some of the blame from H. pylori.
In the modern day USA pills are popped like candy used to. It is strange how scared people are of sugar, gluten and vaccines, while dropping pain killer pills like nothing. Nonsteroidal Anti-inflammatory Drug (NSAIDs) are some of the most common drugs used and comprise many known painkillers (like ibuprofen, diclofenac and aspirine). They inhibit certain enzymes, the cyclooxygenase enzymes (Cox). They also affect the stomach and increase the risk of stomach ulcers. They are the most common cause of peptic ulcers if H. pylori infection is not present. So stop blaming H. pylori for your gastric ulcer when you drop ibuprofen every time you have a hang over.
As with all my posts, there is much more to be said. I did not talk too much about medical treatment of H. pylori, or how garlic could help a little bit (see one of my previous posts here). I wanted to show that doctors do struggle and risk things in order to improve treatment for patients. Dr. Marshall is a good example of a doctor who cares more about finding a cure than about his personal wealth or confort. I also wanted to show that it is not always pathogens, but often times our own senseless abuse of medicine. You cannot blame doctors for your non-responsible use of pain relievers.
Most of all I wanted to explain how stomach ulcers can develop and how H. pylori is involved in it. Microbiology is a very interesting topic. And the more we learn about microbes, the clearer it becomes that a human is only an apobiont (incomplete organism). Generally scientists refer to humans as "holobionts" because there are at least equally as many bacterial cells in and on us as there are human cells. Disease due to bacteria is not due to presence of bacteria, but due to displacement. I mean, S. aureus (one of its strains is responsible for MRSA) lives in and on us. This story, together with these concluding words, hopefully put things a little bit more in perspective. There is never black and white in medicine or science. Just because new results suggest one thing, that does not mean that this is the only thing. So do not listen to the proclaimes of a single solution to disease, because there is none.
Barry Marshall
- Facts, Nobelprize.org - Link
- Biographical, Nobelprize.org - Link
- Wikipedia - Link
- UNIDENTIFIED CURVED BACILLI IN THE STOMACH OF PATIENTS WITH GASTRITIS AND PEPTIC ULCERATION - Link
Peptic Ulcer Frequency
- Frequency and risk factors of gastric and duodenal ulcers or erosions in children: a prospective 1-month European multicenter study - Link
- Peptic ulcer frequency differences related to h. Pylori or aines - Link
- Peptic Ulcer Disease - Link
- NHS inform: Stomach ulcer - Link
- NHS: Stomach ulcer - Link
- Wikipedia: Peptic ulcer disease - Link
- Lehrbuch der Inneren Medizin; Siegenthaler, Kaufmann, Hornborstel, Waller
Dietary Effects
- How diet and lifestyle affect duodenal ulcers. Review of the evidence - Link
- Role of dietary polyphenols in the management of peptic ulcer - Link
- Mayo clinic: Peptic ulcers - Link
- NHS: Stomach ulcer - Link
Stress
- Stress controversies: post-traumatic stress disorder, hippocampal volume, gastroduodenal ulceration - Link
- Self-Perceived Stress and the Risk of Peptic Ulcer DiseaseA Longitudinal Study of US Adults - Link
- Stress and peptic ulcer: life beyond helicobacter - Link
- Lifestyle, Stress, and Genes in Peptic Ulcer DiseaseA Nationwide Twin Cohort Study - Link
General Physiology And Medical Terminology
- Lehrbuch der Inneren Medizin; Siegenthaler, Kaufmann, Hornborstel, Waller
- Human Physiology: From Cells to Systems; Sherwood
- Psychyrembel: Klinisches Wörterbuch; de Gruyter
General Information About H. Pylori And Gastric Ulcers####
- Hypothesis: The Changing Relationships of Helicobacter pylori and Humans: Implications for Health and Disease - Link
- Helicobacters are indigenous to the human stomach: duodenal ulceration is due to changes in gastric microecology in the modern era - Link
- Not all Helicobacter pylori strains are created equal: should all be eliminated? - Link
- Nonsteroidal Anti-inflammatory Drugs and Peptic Ulcer Disease - Link
NSAIDs

I hope you enjoyed this post. Please feel free to share your opinions in the comments. Again, be friendly or stay away. I would love if we could start a similar conversation as in my previous post.
As always,
Cheers @lesshorrible!

I have never suffered from an ulcer in my stomach, and I am one of those who always have ibuprofen around in case I needed it.
Can the presence of H. pylori be called an infection? Considering, it's in more than 50% of the world population and it can even have benefits?
And about the doctor, I like the fact he used himself for his experiment, that means he was no joking around.
Yes, just because ibuprofen can cause stomach ulcers, does not mean it will. NSAIDs are a scientifically accepted risk factor for stomach ulcers.
It is more the colonization and the resulting endotoxins. I did a quick search on the internet and H. pylori could be called an infectious agent. I will need to check one of the clinical books but they are out of reach right now.
There are other bacteria that are found in almost all of us that perform important tasks in our digestive system. If they leave the area where they normaly colonize in the body, they can cause disease. There is a specific term for this, it is bio...., but I forgot the exact term. This is also something I can check tomorrow.
I am sorry that I could not answer your questions in detail, but I will get back to you in the morning. Thank you for your engaging comment though!
What is your take? Do you think H. pylori could be considered an infection?
Cheers!
Congratulations @lesshorrible! You have completed the following achievement on Steemit and have been rewarded with new badge(s) :
Click on the badge to view your Board of Honor.
If you no longer want to receive notifications, reply to this comment with the word
STOPDo not miss the last post from @steemitboard:
SteemitBoard World Cup Contest - Brazil vs Belgium
Participate in the SteemitBoard World Cup Contest!
Collect World Cup badges and win free SBD
Support the Gold Sponsors of the contest: @good-karma and @lukestokes
https://steemit.com/news/@bible.com/6h36cq
@lesshorrible Thank you for not using bidbots on this post and also using the #nobidbot tag!