UNDERSTANDING DIABETES

Source: @Pixabay
DIABETES
Diabetes is a major cause of blindness, kidney failure, heart attacks, stroke and lower limb amputation.
Diabetes is a disease of the pancreas, an organ that produces the hormone called insulin. While health care providers do not yet know what causes diabetes, certain factors can increase a person’s chance of getting diabetes.
Since it is a disease that prevents our body from properly using the energy from the food we eat, diabetes occurs in one of the following situations:
•The pancreas produces little insulin or no insulin at all.
•Insulin is available but does not work as it should (insulin resistance).
When we eat or drink, most of our food is broken down into a simple sugar called glucose. Glucose provides the energy your body needs for daily activities this process is called metabolism. Our body is made up of millions of cells. To make energy, the cells need food in a very simple form.
The blood vessels and blood are the highways that transport sugar from where it is either taken in the stomach or manufactured in the liver to the cells where it is used by our muscles or where it is stored (as fat). The pancreas releases insulin into the blood, which serves as the helper that lets sugar absorbed into the cells for use as energy, since sugar cannot go into the cells by itself.
Once sugar leaves the bloodstream and enters the cells, the blood sugar level is lowered. But when insulin is not available or not working well, sugar cannot get into the body's cells for use as energy. This causes sugar to rise. Too much sugar in the blood is called "hyperglycemia" (high blood sugar) or diabetes.

Source: @Pixabay
SITUATIONS AND TRENDS
Diabetes prevalence has been rising more rapidly in middle- and low-income countries.
WHO estimates that 347 million people worldwide suffer from diabetes. In the region of Africa, around 20 million are living with diabetes. This figure is expected to double by 2030. In comparison to other world regions, Africa has the highest percentage of undiagnosed diabetes cases reaching 62% and the lowest diabetes related health expenditure.
Globally, an estimated 422 million adults are living with diabetes mellitus, according to the latest 2016 data from the World Health Organization (WHO). Diabetes prevalence is increasing rapidly; previous 2013 estimates from the International Diabetes Federation put the number at 381 million people having diabetes. The number is projected to almost double by 2030. Type 2 diabetes makes up about 85-90% of all cases. Increases in the overall diabetes prevalence rates largely reflect an increase in risk factors for type 2, notably greater longevity and being overweight or obese.
Diabetes mellitus occurs throughout the world, but is more common (especially type 2) in the more developed countries. The greatest increase in prevalence is, however, occurring in low- and middle-income countries including in Asia and Africa, where most patients will probably be found by 2030. The increase in incidence in developing countries follows the trend of urbanization and lifestyle changes, including increasingly sedentary lifestyles, less physically demanding work and the global nutrition transition, marked by increased intake of foods that are high energy-dense but nutrient-poor (often high in sugar and saturated fats, sometimes referred to as the Western pattern diet). The risk of getting type 2 diabetes has been widely found to be associated with lower socio-economic position across countries.
The WHO estimates that diabetes resulted in 1.5 million deaths in 2012, making it the 8th leading cause of death. However another 2.2 million deaths worldwide were attributable to high blood glucose and the increased risks of associated complications (e.g. heart disease, stroke, kidney failure), which often result in premature death and are often listed as the underlying cause of death certificates rather than diabetes.
Almost half of all deaths attributable to high blood glucose occur before the age of 70 years. WHO projects that diabetes will be the seventh leading cause of death in 2030.
The prevalence of diabetes in the Philippines is increasing. Rapid urbanization with increasing dependence on electronic gadgets and sedentary lifestyle contribute significantly to this epidemic. Diabetes care in the Philippines is disadvantaged and challenged with respect to resources, government support, and economics. The national insurance system does not cover comprehensive diabetes care in a preventive model and private insurance companies only offer limited diabetes coverage. Thus, most patients rely on “out-of-pocket” expenses, namely, laboratory procedures and daily medications. Consequently, poor pharmacotherapy adherence impairs prevention of complications. Moreover, behavioral modifications are difficult due to cultural preferences for a traditional diet of refined sugar, including white rice and bread.
Non-communicable diseases (NCD; non-infectious or non-transmissible diseases)—including diabetes—in the Philippines account for 6 of the top 10 causes of mortality and are considered a major public health concern. Diseases of the heart and vascular system continue to be the leading causes of death, comprising 31% of all deaths. Other NCDs include malignant neoplasms, chronic obstructive pulmonary disease, and chronic kidney disease. What is alarming is that as deaths due to preventable diseases have been on a decline, lifestyle-related diseases due to “Westernization” of the culture have begun to dominate as the leading causes of death, particularly due to cardiovascular diseases, malignant neoplasms, diabetes, and chronic lower respiratory diseases.
At present, there are no published nationwide prevalence or incidence studies on type 1 diabetes (T1D). However, 1 survey was done in a municipality of Bulacan in Central Luzon Region that showed a very low prevalence of T1D with only 7 cases diagnosed among children aged 0 to 14 years during a 10-year period from 1989 to 1998. A recent survey on pediatric type 2 diabetes (T2D) in the Philippines also found a low prevalence at 0.91%. As a result of the low prevalence of T1D, continuous glucose monitoring (CGM) devices and continuous subcutaneous insulin infusion (insulin pumps) are not widely used. Standard home glucose monitoring devices are readily available and affordable as well as various insulin preparations that are generic and biosimilar via subcutaneous injections. There is little research on stem cell therapy or islet cell transplantation for T1D in the Philippines.
Gestational diabetes (GDM) is prevalent in the Philippines. Published data from the Asian Federation of Endocrine Societies Study Group on Diabetes in Pregnancy (ASGODIP) showed that the Philippines has a GDM prevalence of 14% in 1203 pregnancies surveyed. Because of this high prevalence rate, the Unite for Diabetes Clinical Practice Guideline (CPG) recommends universal GDM screening for the Filipino population. The ASGODIP data found that about 40.4% of high-risk women were positive for GDM when screening was performed beyond the 26th week of pregnancy. In a cohort of Filipino women with GDM delivering babies with macrosomia in the Cardinal Santos Medical Center, >75% were diagnosed between gestational weeks 26 and 38. In another cohort population from the Veterans Memorial Medical Center, 50% of GDM cases were diagnosed between gestational weeks 31 and 40. The Filipino CPG recommends adopting the criteria by the International Association of Diabetes & Pregnancy Study Groups for interpretation of the 75-g oral glucose tolerance test as GDM screening.
T2D is the most common type of diabetes in the Philippines. In 2009, a cohort study derived from the larger population-based investigation in 1998 was revisited and demonstrated a 9-year incidence rate of T2D in the Philippines to be around 16.3%. In the latest survey published by the Food and Nutrition Research Institute in the Philippines (the Eighth National Nutrition Survey of 2013), the prevalence of high fasting blood glucose based on the World Health Organization criteria of >125 mg/dL for individuals >20 years old was 5.4%, an increase of 0.6%, compared with the same study in 2008. The highest prevalence rate was found among the richest in the wealth index, those living in urban areas, and those in the 60- to 69-year age group in both sexes. These studies show an alarming growth rate of T2D in the Philippines commensurate with an upward trend in worldwide prevalence. In the 2014 prevalence estimates published by the International Diabetes Federation, it is estimated that there are 3.2 million cases of T2D in the Philippines with a 5.9% prevalence rate in adults between the ages of 20 and 79 years. Around 1.7 million people with T2D remain undiagnosed. The estimated cost per person with T2D in 2013 in the Philippines is $205, which is comparable with neighboring countries such as Thailand ($285) and Indonesia.
TYPES OF DIABETES
Source: @Pixabay
Type 1 diabetes
Type 1 diabetes (previously known as insulin-dependent, juvenile or childhood-onset) is characterized by deficient insulin production and requires daily administration of insulin. The cause of type 1 diabetes is not known and it is not preventable with current knowledge.
Symptoms include excessive excretion of urine (polyuria), thirst (polydipsia), constant hunger, weight loss, vision changes, and fatigue. These symptoms may occur suddenly.
Type 2 diabetes
Type 2 diabetes (formerly called non-insulin-dependent, or adult-onset) results from the body’s ineffective use of insulin. Type 2 diabetes comprises the majority of people with diabetes around the world, and is largely the result of excess body weight and physical inactivity.
Symptoms may be similar to those of type 1 diabetes, but are often less marked. As a result, the disease may be diagnosed several years after onset, once complications have already arisen.
Until recently, this type of diabetes was seen only in adults but it is now also occurring increasingly frequently in children.
Gestational diabetes
Gestational diabetes is hyperglycaemia with blood glucose values above normal but below those diagnostic of diabetes, occurring during pregnancy.
Gestational diabetes occurs when there is a high blood glucose level during pregnancy. As pregnancy progresses, the developing baby has a greater need for glucose. Hormone changes during pregnancy also affect the action of insulin, which brings about high blood glucose levels.
Pregnant women who have a greater risk of developing gestational diabetes include those who:
• Are over 25 years old
• Are above their desired body weight
• Have a family history of diabetes
• Are Hispanic, African-American, Native American, or Asian-American.
Blood glucose levels usually return to normal after childbirth. However, women who have had gestational diabetes have an increased risk of developing Type 2 diabetes later in life.
Women with gestational diabetes are at an increased risk of complications during pregnancy and at delivery. They and their children are also at increased risk of type 2 diabetes in the future.
Gestational diabetes is diagnosed through prenatal screening, rather than through reported symptoms.
CAUSES OF DIABETIS
The causes of diabetes are not known. The following factors may increase your chance of getting diabetes:
•Family history of diabetes or inherited tendency
•African-American, Hispanic, Native American, or Asian-American race, Pacific Islander or ethnic background
•Being overweight (20 percent or more over your desired body weight)
•Physical stress (such as surgery or illness)
•Use of certain medications, including steroids and blood pressure medications
•Injury to the pancreas (such as infection, tumor, surgery, or accident)
•Autoimmune disease
•High blood pressure
•Abnormal blood cholesterol or triglyceride levels
•Age (risk increases with age)
•Alcohol (risk increases with years of heavy alcohol use)
•Smoking
•History of gestational diabetes or delivery of a baby weighing more than 9 pounds (4.1 Kg).
•Pregnancy
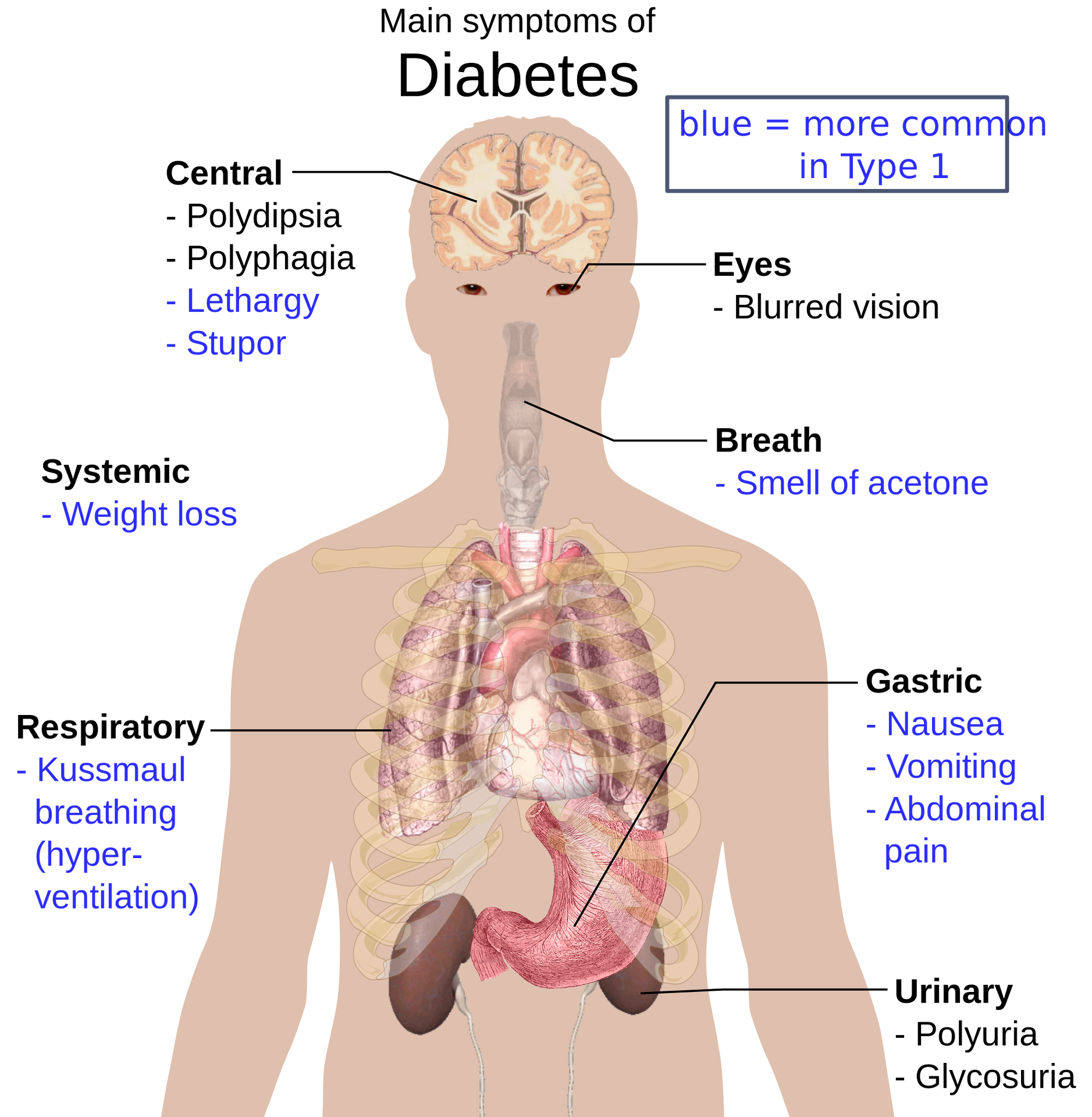
SYMPTOMS OF DIABETES
• Increased thirst
• Increased hunger (especially after eating)
• Dry mouth
• Frequent urination
• Unexplained weight loss (even though you are eating and feel hungry)
• Weak, tired feeling
• Blurred vision
• Numbness or tingling in the hands or feet
• Slow-healing sores or cuts
• Dry and itchy skin (usually in the vaginal or groin area)
• Frequent yeast infections
CONSEQUENCES AND COMPLICATIONS OF DIABETES
Over time, diabetes can damage the heart, blood vessels, eyes, kidneys, and nerves.
•Retinopathy (eye disease): All patients with diabetes should see an ophthalmologist (eye specialist) every year for a dilated eye examination. Patients with known eye disease or symptoms of blurred vision in one eye or who have blind spots may need to see their ophthalmologist more often.
•Nephropathy (kidney disease): Urine testing should be performed every year. Regular blood pressure checks also are important because control of high blood pressure is essential in slowing kidney disease. Generally, blood pressure should be less than 130/80 in adults. Persistent swelling in the leg or feet also may be a symptom of kidney disease and should be reported to your doctor.
•Neuropathy (nerve disease): Numbness or tingling in your feet should be reported to your doctor at your regular visits. Check your feet every day for redness, calluses, cracks, or breakdown in the skin tissue. If you notice these symptoms before your scheduled visits, notify your doctor immediately.
•Adults with diabetes have a two- to three-fold increased risk of heart attacks and strokes.
•Combined with reduced blood flow, neuropathy (nerve damage) in the feet increases the chance of foot ulcers, infection and eventual need for limb amputation.
•Diabetic retinopathy is an important cause of blindness, and occurs as a result of long-term accumulated damage to the small blood vessels in the retina. 2.6% of global blindness can be attributed to diabetes.
•Diabetes is among the leading causes of kidney failure.
DIAGNOSIS OF DIABETES
Early diagnosis can be accomplished through relatively inexpensive testing of blood sugar. Diabetes is diagnosed with fasting sugar blood tests or with A1c blood tests, also known as Glycated Hemoglobin tests. A fasting blood sugar test is performed after you have had nothing to eat or drink for at least eight hours. Normal fasting blood sugar is less than 100 mg/dl (5.6 mmol/l). No fasting required for an A1c blood test.
Diabetes is diagnosed by one of the following:
•Blood sugar level is equal to or greater than 126 mg/dl (7 mmol/l).
•Two random blood sugar tests over 200 mg/dl (11.1 mmol/l) with symptoms.
•An Oral Glucose Tolerance Test (OGTT) with results over 200 mg/dl (11.1 mmol/l).
•Your A1c test is greater than 6.5% on two separate days.
* Normal Pre-diabetes Diabetes*
Fasting Glucose Test--------- Less than 100---------100-125---------126 or higher
Random Glucose Test--------Less than 140---------140-199---------200 or higher
A1c Test--------------------------Less than 5.7%-------5.7 - 6.4%-------6.5% or higher
Source: American Diabetes Association 2010

Source: @Pixabay
MEDICATIONS FOR DIABETES
Class and Drugs
Biguanides- Metformin
Sulfonylureas- Glibenclamide, glipizide, gliclazide, glimipride
α-glucosidase inhibitor- Acarbose
DDP-IV Inhibitors- Sitagliptin, saxagliptin, vildagliptin, linagliptin
GLP1 receptor agonists- Liraglutide, exenatide, lixisenatide
SGLT2 Inhibitors- Dapaglifozin, empagliflozin, canagliflozin [pending]
Insulins- Human Insulin R, Mix 70/30, NPH, glulisine, insulin aspart, detemir, glargine, degludec
DDP-IV, dipeptidyl peptidase-4; GLP1, glucagon-like peptide 1; SGLT2, sodium glucose cotransporter-2

Source: @Pixabay
PREVENTION AND CONTROL OF DIABETES
Treatment of diabetes involves diet and physical activity along with lowering blood glucose and the levels of other known risk factors that damage blood vessels. Tobacco use cessation is also important to avoid complications. There is no cure for diabetes, but it can be treated and controlled. The goals of managing diabetes are to:
1. Keep your blood glucose levels as near to normal as possible by balancing food intake with medication and activity.
2. Maintain your blood cholesterol and triglyceride (lipid) levels as near the normal ranges as possible by decreasing the total amount of fat to 30% or less of your total daily calories, and by reducing saturated fat and cholesterol.
3. Control your blood pressure. (Your blood pressure should not go over 130/80.)
4. Decrease or possibly prevent the development of diabetes-related health problems.

Source: @Pixabay
KEYS TO MANAGE DIABETES:
• Plan what you eat and following a balanced meal plan. Eat a healthy diet, avoid sugar and saturated fats intake.
• Achieve and maintain healthy body weight.
• Exercise regularly. Be physically active – at least 30 minutes of regular, moderate-intensity activity on most days. More activity is required for weight control.
• Avoid tobacco use – smoking increases the risk of diabetes and cardiovascular diseases.
• Take medication, if prescribed, and closely following the guidelines on how and when to take it.
• Monitor your blood glucose and blood pressure levels at home.
• Keep your appointments with your health care providers and having laboratory tests completed as ordered by your doctor.
WHO RESPONSE
World Health Organization aims to stimulate and support the adoption of effective measures for the surveillance, prevention and control of diabetes and its complications, particularly in low and middle-income countries. To this end, WHO:
• provides scientific guidelines for the prevention of major non-communicable diseases including diabetes;
• develops norms and standards for diabetes diagnosis and care;
• builds awareness on the global epidemic of diabetes, marking World Diabetes Day (14 November); and
• conducts surveillance of diabetes and its risk factors.
The WHO "Global report on diabetes" provides an overview of the diabetes burden, the interventions available to prevent and manage diabetes, and recommendations for governments, individuals, the civil society and the private sector.
The WHO "Global strategy on diet, physical activity and health" complements WHO's diabetes work by focusing on population-wide approaches to promote healthy diet and regular physical activity, thereby reducing the growing global problem of overweight people and obesity.
Diabetes Programs in the Philippines
Diabetes awareness campaigns have always been at the forefront of activities among diabetes organization in the Philippines, including the PSEDM, The Institute for Diabetes Foundation (IDSF), Diabetes Philippines (DP), American Association of Clinical Endocrinologists Philippines (AACE Philippines), and the Philippine Center for Diabetes Education Foundation (PCDEF).
Diabetes Awareness month is celebrated every July with concurrent activities nationwide, including many lay forum events. The Department of Health also reserves every fourth week of July in its yearly calendar for a Diabetes Awareness campaign.
Additionally, general practitioners and internal medicine specialists regularly attend diabetes workshops by these organizations to optimize care in underserved regions.
Diabetes care in the Philippines continues to be a challenge for the primary care physicians of the region as urbanization continues to augur a significant rise in disease prevalence over the next few years. Key features of diabetes care in the Philippines are provided in Table 2. The region is expected to have one of the highest number of newly diagnosed diabetes by 2025. Philippine Practice Guidelines on the Diagnosis and Management of Diabetes Mellitus recommends that Filipinos age >40 years and those at risk for developing diabetes should be tested annually owing to the significant prevalence and burden of diabetes.
Key Features of Diabetes Care in the Philippines
• Prevalence of diabetes in the Philippines is increasing due to rapid urbanization and Westernization of the Filipino culture.
• “Out-of-pocket” system of health care continues to be the main mechanism of patient–doctor relationship and compensation.
• The national insurance system does not allow comprehensive coverage of diabetes management, is only limited to certain household members, and provides limited medication coverage.
• Both generics and branded antihyperglycemic medications are readily available including both human and analog insulins.
• Metformin and sulfonylureas are the most commonly prescribed medications due to availability and cheaper cost.
• Individuals with diabetes receive very strong family support.
Fundamental and transformative changes are necessary to increase diabetes awareness, emphasize lifestyle change while respecting cultural preferences, and promoting public policies particularly with the health insurance system, to improve overall diabetes care and outcomes.
Unless both government and private organizations go hand in hand in combatting the spread of this disease, by implementing programs such as limiting fast food advertising in print form and on television, as well as implementing disease awareness campaigns including early detection and financial support for the afflicted underprivileged, it is expected that diabetes will continue to haunt Filipinos in the next century with increasing economic burden not only for individual families but also the entire nation.
Sources:
• http://lifestyle.inquirer.net/225706/the-philippines-is-now-a-diabetes-hotspot/#ixzz4vAe2tycA
• http://www.sciencedirect.com/science/article/pii/S2214999615012643
• https://doi.org/10.1016/j.aogh.2015.10.004
• http://www.who.int/mediacentre/factsheets/fs312/en/
• https://my.clevelandclinic.org/health/articles/diabetes-mellitus-an-overview
Please support @surpassinggoogle as a witness by voting him at https://steemit.com/~witnesses and type in "steemgigs" at the first search box.
You can also give him witness voting decisions on your behalf, visit https://steemit.com/~witnesses again and type in "surpassinggoogle" in the second box as a proxy.
Please support his project as well, which is @teardrops Smart Media Token.
I would like also to thank my #steemunity, #steemph, #teardrops, #steemgigs and #untalented, and #steemitachievers family