Runner's Knee - Iliotibial Band Syndrome
Do you get a burning pain on the outside of your knee when running, cycling or rowing?
On the outside of knee cap and the end of your thigh, you’ll feel a prominent bony bump. This is your “lateral epicondyle”. Is it tender if you put pressure on (or just below) this region?
If you’re experiencing this pain, you may have a condition called ITB syndrome. Your Iliotibial Band (ITB) is strong “band” of fibres that runs down the outside of your thigh and connects to the top of your shin bone (tibia). This, and its underlying structures are the source of pain in ITB syndrome.
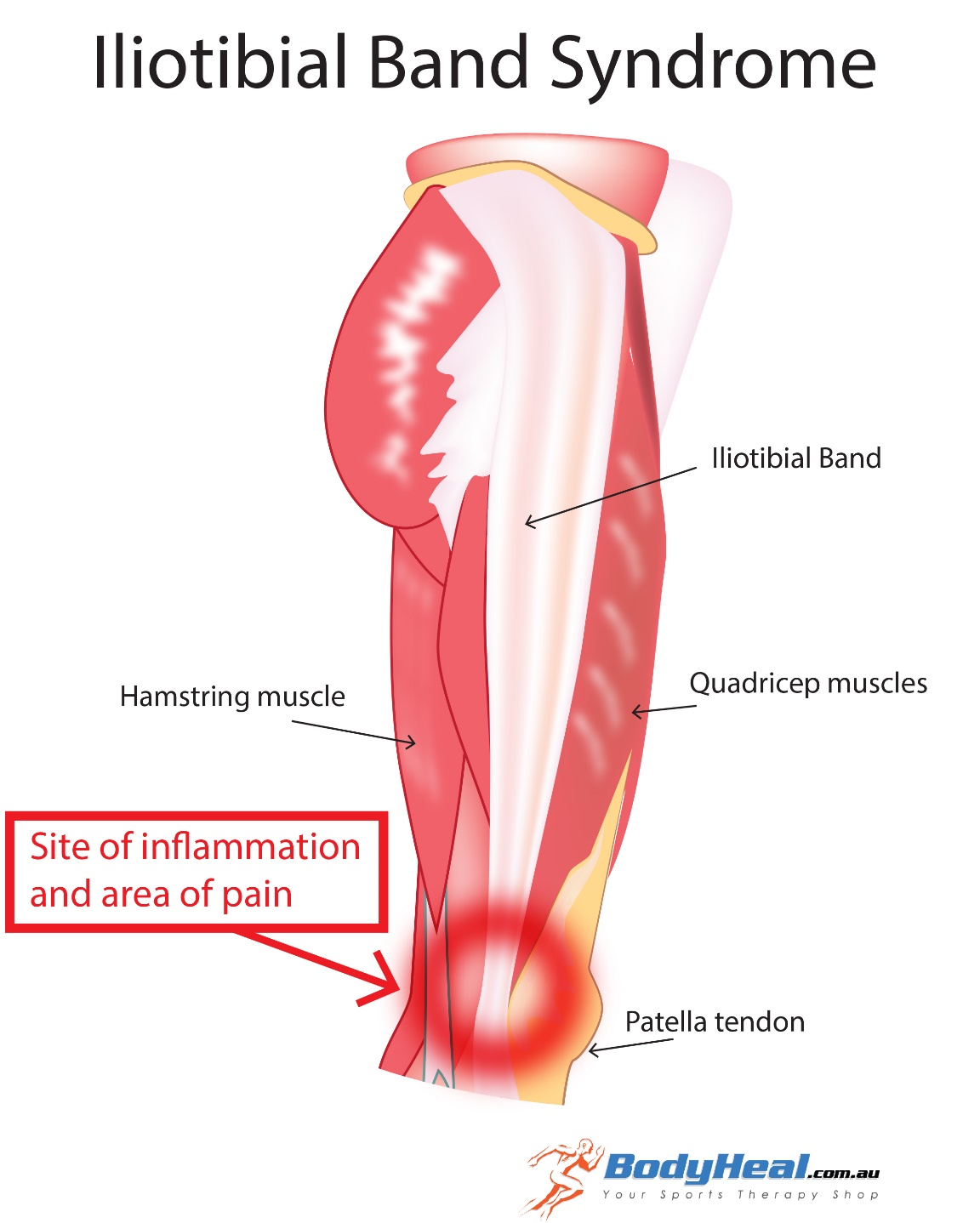
image source: www.bodyheal.com.au
How ITB Syndrome is Diagnosed:
ITB Syndrome is the most running common lateral (outer side) knee injury. It is also very common in cyclists. Women are more affected than men.
Your physiotherapist can diagnose ITB syndrome via the following tests:
- Renne’s and Noble’s Tests
- Observation for Trendelenburg’s sign
- Pain when bending the knee
- Strength of Gluteal Muscles
Medical imaging generally not needed, but can help to identify the extent of the injury in chronic cases, and rule out other conditions that cause similar pain.
Causes of ITB Syndrome:
It is agreed that ITB Syndrome is an overuse injury that causes pain around the lateral epicondyle, and it is due to activities that require repeated bending of the knee (such as running). However, the actual source of the pain is still under debate.
The original theory, which is still widely accepted today, is the pain caused by friction, or constant rubbing of the ITB against the lateral epicondyle, causing irritation and chronic inflammation of the ITB and the underlying structures. Hence it is often referred to as ITB Friction Syndrome.
However, recent research and careful study of the anatomy has suggested that friction is not the mechanism of injury, but rather it’s the repeated compression of the structures that sit between the ITB and the lateral epicondyle that causes them to become irritated and painful.
Regardless of the theory behind the injury, there is consensus that ITB Syndrome is associated with weak gluteal muscles that lead to suboptimal biomechanics at the hip, which flow onto the knee.
Other factors that are thought to cause ITB syndrome are ITB tightness, excessive over-pronation of the foot and increased knee flexion during movement, but these claims are questionable, with not a lot of evidence to support them.
Treatment of ITB Syndrome:
If you’re experiencing any knee pain, the first step is to stop or reduce the activity that’s causing the pain (e.g. running) and seek professional advice for a proper diagnosis and strategy to manage the condition.
The majority of patients report good outcomes with conservative treatment. Your physiotherapist can help you in reducing pain and resolving ITB Syndrome through the following strategies:
- Fascia and trigger point release with massage and dry needling/acupuncture
- Strengthening of the gluteal muscles
- Retraining the control of the muscles around the hip
- Improving your running technique
For pain relief, the RICE (rest, ice, compression and elevation) principle can be effective. Corticosteroid injections have also been shown to be very effective for early pain relief, but caution must be taken as the use of these pharmaceuticals has been associated with delayed tissue healing and poorer long term outcomes.
References:
Demol, Y., & Ackerman, A. (2016). Iliotibial Band Syndrome Retrieved December 05, 2016, from http://www.physio-pedia.com/Iliotibial_Band_Syndrome
Ellis, R., Hing, W., & Reid, D. (2007). Iliotibial band friction syndrome—A systematic review. Manual Therapy, 12(3), 200-208. doi: http://dx.doi.org/10.1016/j.math.2006.08.004
Fairclough, J., Hayashi, K., Toumi, H., Lyons, K., Bydder, G., Phillips, N., . . . Benjamin, M. (2007). Is iliotibial band syndrome really a friction syndrome? Journal of Science and Medicine in Sport, 10(2), 74-76. doi: http://dx.doi.org/10.1016/j.jsams.2006.05.017
Renne, J. W. (1975). The iliotibial band friction syndrome. The Journal of Bone & Joint Surgery, 57(8), 1110.