Real clinical history: "Malaria"

Figure 1. Mosquito that causes malaria.
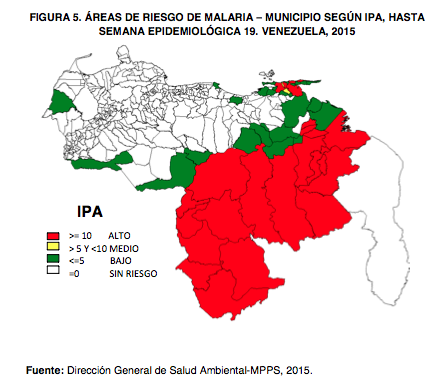
Figure 2. Risk areas in Venezuela data provided in 2015. The red zone are those where the mosquito (jungle areas) is more abundant. Data provided by the environmental health directorate in venezuela.
Although it seems a little illogical in recent years has become frequent malaria infections or also called malaria, in my country Venezuela that has a variety of wild areas with tropical climate have determined certain endemic areas like the states: Bolivar, Amazonas , Delta Amacuro, Monagas and Zulia. Although I am currently in the state of Trujillo withdrawn from the areas already named, it has become common to diagnose people with this disease, the last one diagnosed a week ago was a young male of 27 years of age with no pathological history , known who started his current illness for more than 15 days characterized by headache, malaise, asthenia, mild abdominal pain, chills and fever quantified at 39 and 40 ° C, so he went to the local medication and is treated as a viral process, then as the zika virus in view of the persistent symptoms decides to go to the hospital where it is valued. At physical examination he was a patient in regular clinical conditions, febrile at rest, dehydrated, eupneic, with icteric skin and mucous dye, stable cardiopulmonary soft abdomen depressing painful on palpation in the left hypochondrium, with significant splenomegaly with touch of the neurological state. Vital signs blood pressure 90/60 heart rate 76'm respiratory rate 17'mint with a paraclinica q leucositosis at the expense of segmented, moderate anemia and impaired hepatic function.
In view of the clinical conditions he presents, his income is determined. During the interrogation, the young man tells us that he made a trip about two weeks ago to Bolivar, where he lasted a couple of days in a jungle area. He started treatment with antibiotic therapy, hydration parenteral, antipyretic, coproanalysis, uroanalysis, thorax Rx, pelvic abdominoid, serology for dengue, cytomegalovirus, febrile antigens, blood culture, etc. After a couple of days we received the results where the positive with this patient was that the parasite P vivax had been isolated in one of the samples taken. The next step was to notify the case to epidemiology who values and starts treatment with antimalarial drugs, currently said patient is receiving treatment and in control by the service.
A few days later, a close relative arrived with the same symptomatology, but never traveled to endemic areas, always remained in an area of origin, which is isolated in the same parasite in blood. Although Trujillo is not an epidemiological area for malaria in recent years, it takes great importance and prevalence for the isolation of this disease.
In the world for now there are 4 species of the genus Plasmodium, (etilogical agent) that affect the human being and these are:
-P. Vivax
-P. Ovalae
-malarae
-P. Falciparum (the latter causes most of the recorded deaths from malaria).
Although malaria is not one of the most common parasitic diseases in humans and has been isolated in all tropical regions of the world, this disease is transmitted by the bite of the anopheles mosquito.
Now, as is the pathogenesis of this infection in the human being;
It all starts with the mosquito bite which inoculates the sporozoites from the salivary glands of the animal into the man's bloodstream, after a period of asexual reproduction in the hepatocytes, the cells that are swollen burst and release the merozoites into the bloodstream, and this is where the symptomatic phase of infection begins.
These merozoites bind to specific receptors on the surface of the hematies and then penetrate into them, after invading the hematies, the parasite grows more and more, consuming and degrading the intracellular proteins (mainly hemoglibin) and injuring the cell membrane.
In most pathologies the host defenses play a very important role and in this process is not the exception, in nonimmune people, said infection awakens nonspecific defense mechanisms such as the filtration function exerted by the spleen.
When the parasitized hematies that have eluded the splenic filter rupture, the released material activates the macrophages and causes them to release inflammatory cytokines, which produce fever and other pathological effects.
Repeated contacts with malaria cause a specific immune response that reduces the intensity of parasitaemia. Over time, patients become immune to the disease, but remain vulnerable to infection.
Once described all the pathophysiology in the human organism and the replication of the parasite in the same, you can expose and understand all the symptomatology and these are:
nonspecific symptoms; malaise, headache, asthenia, abdominal pain, fever, chills, vomiting and nausea.
-Hosting orthostatic
It is necessary to take into account that in the beginning the fever is usually irregular, usually occurs with anemia and splenomegaly.
Malaria complications include: cerebral malaria, hypoglycemia, lactic acidosis, noncardiogenic pulmonary edema, renal insufficiency, disseminated vascular coagulation and aspiration pneumonia.
The diagnosis of this pathology is quick and simple and consists in demonstrating the presence of the asexual forms of the parasite in the smears of peripheral blood, either in thin or thick extensions, held in Giemsa. The intensity of the parasitemia can be determined in both types of smears and is expressed in number of erythrocytes parasitized by 1000 cells. Its histological characteristics in the smears are double chromatin granulations (infection of many hematies of normal size) gametocytes in the form of banana and parasitemia superior to 5%.
It exits the antimalarial treatment where the drug of choice are quinidine in this case CHLOROQUIN at doses of 10kg / kg kg every 8 hours.
As a prophylactic measure are drugs such as MEFLOQUIN 250mg orally once a week, DOXICYCLIN 100mg orally once a day and lastly CHLOROQUIN 500mg orally once a week.
It is necessary to take into account that in patients in the acute and symptomatic phase of the illness that receive antimalarial drugs should also receive anticomisial drugs such as phenobarbital (dose only 5 to 20mg / kg weight) to avoid seizures. Blood glucose tests should be requested every 6 to 4 hours and those patients with hypoglycemia with values equal to or lower than 40mg / dL should receive EV dextrose test.
Source figure 1: http://www.mirror.co.uk/lifestyle/health/what-malaria-symptoms-treatments-how-8656227
Source figure 2: http://2016.transparencia.org.ve/2015-puede-cerrar-con-130-mil-casos-de-malaria/
Author source: Harrison. (2004). Principios de medicina interna. Decima Quinta edicion. Madrid. Editorial Mc graw Hill, pag 522 y 523.
The content was prepared by myself with help in the theory about the disease of the book already mentioned.
As advice and prevention for malaria always recommend not leaving stagnant water ie bottles, containers, rubbers, masks among others. When you feel some of the symptoms, you should immediately go to the nearest medical center. Remember that malaria is very easy to prevent but it is also easy to get the disease.
By: Johana Albarran
Doctor