Operating: A nail to the tibia

Tibial Surgery
Today I had an operating room day where things went well, and where every day I prepare myself for the final moment of my trip where I will finish learning everything necessary.
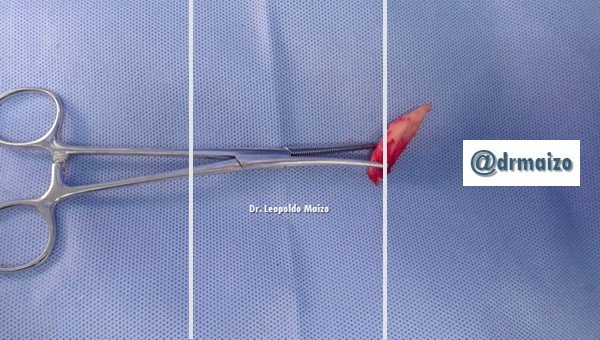
Fractures of the tibial diaphysis (breakage of the bone in the long middle section of the tibia) are caused in most cases by high-energy trauma such as car accidents. One commonly used method of fixation is intramedullary nailing. This method involves inserting a metal rod, usually from the upper side of the tibia, into the internal cavity (medulla) of the tibia. The rod is usually held in place with screws. One widely available and used surgical technique for placing intramedullary nails is the insertion of intramedullary nails with reaming (the bone cavity is reamed before inserting the nail into the space of the bone cavity) or without reaming.

Tibia
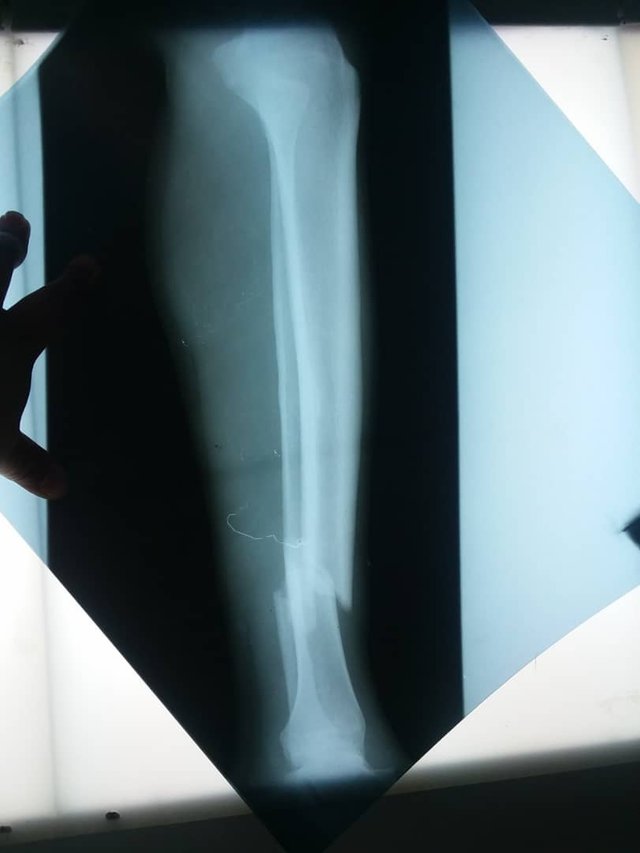

The tibia, being a hypodermic bone in its anterior face, is especially vulnerable to traumatic injuries, its fractures being very common. Its incidence in the Indian subcontinent is 70.000-80.000 per year. If not treated properly, a wide variety of complications can occur: infection, pseudoarthrosis, vicious consolidation, stiffness of the knee or ankle, etc.
There is a great diversity of treatments available, including orthopedic treatment with plaster, osteosynthesis with plate (neutralization, compression), intramedullary nailing with or without lock, Ender nailing, Illizarov circular external fixation, monolateral external fixation, etc. Each modality has advantages and disadvantages, but above all it has its indications. The external fixation has its clear indications in open fractures or of great comminution; however, the intramedullary interlocking system has demonstrated, in general, to have the best results, existing great variety of designs of nails available in the world.



Tibial Fracture
Diaphyseal fractures of the tibia continue to be the most common fractures of the long bones; and of these most are closed as shown by Court-Brown who found 76.5% of closed fractures, related to low energy events.
For the treatment of these fractures there is the conservative treatment (plaster apparatus) and the surgical treatment, which is of our interest. There are several modalities, which include dynamic compression plates which are always placed opening the fracture focus; external fixators that after consolidation need the removal of the fracture and support with the use of plaster appliances, and intramedullary nails milled.
With respect to milled intramedullary nails, there are a number of conditions that indicate a certain disadvantage with respect to UTN (unreamed) nails; however, these are still controversial.
Some authors mention that the drilling procedure produces a greater bleeding and a prolonged operative time. In addition, the point where the detractors of this method do more impetus is the alteration of the endostic circulation as demonstrated by Klein et al, who found a 70% decrease in cortical blood flow with drilling compared to a decrease of 30% without drilling; this would occur because drilling would increase intramedullary pressure, occlude blood vessels by fatty plungers and bone detritus along with thermal damage.
There are also other disadvantages such as possible bone and dermal necrosis, as a consequence of the high temperature generated by drilling exceeding 100°C intramedullary; according to Berman et al an obvious cellular necrosis occurs with temperatures above 70°C; and this of course could lead to osteomyelitis.
The alteration of the vascularization mentioned above could also produce defects in the consolidation process as well as infection.
After all these antecedents we give place in our article to the use of the unreamed intramedullary nail (UTN); this is a rigid nail that allows to be blocked distally with the help of the DAD without the need of intensifier of images, in addition the proximal block through its elliptical hole allows micromovements at the level of the fracture that favors the formation of the bony callus, this is made when radiologically there is presence of fibrous callus, the static screw is removed and the patient begins to support without need of plaster.

The most important thing we can say is that the unreamed Intramedullary Nail is a good alternative in the surgical treatment of diaphyseal fractures of tibia both closed and exposed of 1st degree, as well as in pseudoarthrosis and we affirm this on the basis that the solid nail allows the reduction of the fracture to closed sky achieving the consolidation of the fracture in an average of 16 weeks.
Finally, due to the early onset of joint movement, no joint stiffness or muscular atrophy is observed.

If you need recommendations or help in orthopedic surgery and traumatology do not hesitate to contact me.
Dr. Leopoldo Maizo - Orthopedic Surgeon
If you want to read more I invite you to visit my page:

Firma diseñada por @themonkeyzuelans, contáctalos vía Discord "themonkeyzuelans#9087"
Great projects from the Steemit community:
- My Fundition campaign: https://fundition.io/#!/@drmaizo/6f88ggj8h


.png)
This project is being supported by @Fundition
Fundition is a next-generation, decentralized, peer-to-peer crowdfunding and collaboration platform, built on the Steem blockchain.
#upfundition and #fundition tags on Steem represent the projects that are started on https://fundition.io.
Are You Prepared to Make the World a Better Place too?
Read the full details of Fundition Fund program
Learn more about Fundition by reading our purplepaper
Join a community with heart based giving at its core